David Baxter PhD
Late Founder
Diagnosing and treating interstitial cystitis
Harvard Women's Health Watch
August 2011
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate ? sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel
syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).
There's no cure for IC, but many treatments offer some relief, either singly or in combination. Figuring out what works can be hit-or-miss; there's no way to predict who will respond best to which treatment. Fortunately, increasing awareness and greater understanding of this complex disorder are helping to speed diagnosis and encourage research. In March 2011, the American Urological Association (AUA) issued its first set of guidelines for the diagnosis and management of interstitial cystitis/painful bladder syndrome. (A summary was published in the June 2011 Journal of Urology; the complete guidelines are available here: www.health.harvard.edu/ic_guidelines.) Also, the Agency for Healthcare Research and Quality (a federal research group that reviews what does and doesn't work in health care) is preparing a report on the effectiveness of treatments for chronic pelvic pain in women, including IC; the final report is expected in late 2011, but a draft is available here: www.health.harvard.edu/ic_report.
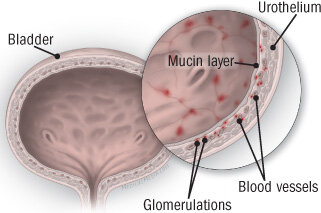
A defect in the layer of mucus (mucin layer) that protects the cells lining the bladder (the urothelium) may permit toxic substances from urine to seep through and inflame tissues. Irritated blood vessels produce tiny areas of bleeding in the bladder lining called glomerulations. Most people with interstitial cystitis have glomerulations.
Possible causes
No one knows the exact cause of IC; more than one mechanism is probably involved. Biopsies of the bladder wall in people with IC indicate various abnormalities, but it's not clear whether these are the cause of the condition or the result of some other underlying process. Some research has focused on defects in the glycosaminoglycan (GAG) layer, part of the layer of mucus that lines and protects the bladder. Defects in the GAG layer may allow toxins in the urine to leak through and damage underlying nerve and muscle tissues; this in turn may trigger pain and hypersensitivity.
Another line of research centers on antiproliferative factor (APF), a substance that's found only in the urine of people with IC. APF appears to block the normal growth of cells that line the bladder and may hinder the healing process that follows any damage or irritation to bladder tissues. Scientists seeking a diagnostic test for IC are considering APF as a possible
biomarker.
There are several other theories about the cause of IC. It may be an infection with an unknown agent, such as a virus. Or it may be an autoimmune disorder set in motion by a bladder infection. It's possible that mast cells normally involved in allergic responses are releasing histamine into the bladder. Another idea is that sensory nerves in the bladder somehow "turn on" and spur the release of substances that contribute to symptoms. Because interstitial cystitis is mainly a woman's disease, many researchers think that hormones play a role.
Variable symptoms
The onset of IC is usually gradual, with bladder pain and urinary urgency and frequency developing over a period of months. The course of the disorder and its symptoms can vary greatly from woman to woman and even in the same woman. Symptoms may change from day to day or week to week, or they may remain constant for months or years and then go away, only to return several months later. Pain ranges from dull and achy to acute and stabbing; discomfort while urinating fluctuates from mild stinging to burning. But virtually everyone with IC has pain associated with bladder filling and emptying. Some women with IC have a constant need to urinate, because urinating helps relieve the pain.
In women who also have chronic abdominal or pelvic pain from other causes, such as irritable bowel syndrome or endometriosis, IC may flare up when those symptoms are at their worst. Sexual intercourse can trigger pain lasting several days, and symptoms may worsen with menstruation. On the other hand, some women experience complete relief during the second and third trimesters of pregnancy. Some find that their symptoms are worse after consuming certain foods or drinks, including strawberries, oranges, tomatoes, chocolate, spices, caffeine, alcohol, and beverages that acidify the urine, such as cranberry juice.
Diagnosis of exclusion
IC is not a urinary tract infection, and it can't be identified by a simple urinalysis or urine culture. Rather, it's a diagnosis of exclusion, which means that it's diagnosed only after a number of other conditions have been ruled out. A clinician ? usually a urologist or a gynecologist ? will first take a thorough history, then conduct a physical exam (including a pelvic exam, if it's not too uncomfortable) and perform tests for infection, bladder stones, bladder cancer, kidney disease, multiple sclerosis, endometriosis, sexually transmitted diseases, and other disorders. The AUA guidelines also recommend an early assessment of pain, urinary frequency, and urine volume, to help evaluate the effectiveness of later treatments.
If a diagnosis is uncertain or there are symptoms (such as blood in the urine) that suggest other problems, the next step is usually cystoscopy, which involves inserting a fiber-optic tube through the urethra to look at the bladder wall. During the procedure, a tissue sample may be taken to rule out bladder cancer. Some clinicians favor hydrodistention under local or regional anesthesia, which involves filling the bladder during cystoscopy with a liquid that stretches it, providing a closer view of the bladder wall. However, AUA guidelines do not recommend hydrodistention for either diagnosis or treatment. In people with IC, glomerulations ? tiny pinpoint spots of blood ? are usually visible on the bladder wall during cystoscopy with hydrodistention, but these lesions are often seen within the normal bladder as well.
One finding from cystoscopy that can help in making an IC diagnosis is the presence of reddened patches or lesions called Hunner's ulcers, which can stiffen tissue and cause reduced bladder capacity. However, Hunner's ulcers, which occur in 10% to 15% of cases, aren't required to make an IC diagnosis.
The potassium sensitivity test, which involves instilling potassium chloride into the bladder to see if it triggers pain, has been proposed for use in diagnosing IC, but it's not conclusive and the AUA does not recommend it for routine use.
Managing IC
There's little consensus on the best way to treat IC, but treatment generally starts with conservative measures and proceeds to more invasive ones if symptoms don't improve. Usually a combination of approaches is needed, including
these:
Psychosocial support. Chronic pain can be an isolating experience, so it may help to be in touch with others who feel your pain and understand what you're going through. Local pain support groups or national support groups like the Interstitial Cystitis Association (see "Selected resources") can serve that purpose. Learning as much as you can about
IC may also give you a greater sense of control over your condition. Chronic pain can cause depression, so don't hesitate to consult a mental health professional if you're feeling overwhelmed. (Support groups can usually refer you to counselors.) You may also want to talk to someone who specializes in stress reduction techniques, such as guided imagery, which was shown in one controlled study to improve IC patients' response to therapy. Some people say
they've been helped by biofeedback, which trains people to use their minds to control physiological processes, such as muscle tension, that may be contributing to symptoms.
Behavior changes. Avoid anything that appears to cause flare-ups, whether that's a certain kind of exercise, sexual activity, constipation, tight clothing, or a specific food. (Because high-acid foods seem to cause flare-ups, some clinicians suggest taking an antacid with meals.) Expanding your bladder capacity is also important (constantly succumbing to the
urge to go all the time can shrink bladder capacity). For example, if you're urinating every 30 minutes, try holding off for 45 minutes; if you manage that for a week, increase the interval to 60 minutes the second week, and so forth.
Medications. Various medications may help relieve pain and reduce inflammation. (See "Medications for the treatment of interstitial cystitis.") Some are taken orally; others are bladder instillations ? drugs that are introduced into the bladder by catheter and held for a few seconds up to 10 or 15 minutes. Instillation usually takes place in a clinician's office, although in some cases, these drugs can be self-administered at home.
Specialized physical therapy. Working with a physical therapist trained in pelvic soft tissue manipulation and rehabilitation may help to release scars and other sources of pelvic pain. Exercises that relax the pelvic floor are okay, but the AUA recommends that people with IC avoid exercises that strengthen pelvic floor muscles (Kegels).
Additional options. If standard treatments don't work, your clinician may suggest a trial of an implantable device called InterStim, which stimulates the sacral nerve in the lower back and may help alleviate urinary urgency and frequency in some women. If the device helps, it can be permanently implanted. Researchers are also studying the instillation of botulinum toxin into the bladder, but so far, the side effects and complications have been too serious to recommend its general use.
What doesn't work. The AUA found no evidence that the following therapies help relieve IC symptoms, and some evidence they may be harmful: long-term oral antibiotics, bladder instillation of bacillus Calmette-Guerin (BCG), and bladder instillation of resiniferatoxin (RTX).
Dr. Kathy Niknejad, Director of Surgical Specialties at Harvard Vanguard Medical Associates in Boston and instructor in surgery at Harvard Medical School, helped prepare this article.
Selected resources
American Urological Association Foundation
800-828-7866 (toll-free)
www.urologyhealth.org
Interstitial Cystitis Association
800-435-7422 (toll-free)
www.ichelp.org
Interstitial Cystitis Network
707-538-9442
www.ic-network.com
Harvard Women's Health Watch
August 2011
Also called painful bladder syndrome, this frustrating disorder disproportionately affects women.
Interstitial cystitis is a chronic bladder condition that causes recurring bouts of pain and pressure in the bladder and pelvic area, often accompanied by an urgent and frequent need to urinate ? sometimes as often as 40, 50, or 60 times a day, around the clock. Discomfort associated with interstitial cystitis can be so excruciating that, according to surveys, only about half of people with the disorder work full-time. Because symptoms are so variable, experts today describe interstitial cystitis as a member of a group of disorders collectively referred to as interstitial cystitis/painful bladder syndrome. (In this article, we'll call it interstitial cystitis, or IC.)
Among the one to two million Americans with IC, women outnumber men by as much as eight to one, and most are diagnosed in their early 40s. Several other disorders are associated with IC, including allergies, migraine, irritable bowel
syndrome, fibromyalgia (a condition causing muscle pain), chronic fatigue syndrome, and vulvodynia (pain or burning in the vulvar area that isn't caused by infection or skin disease).
There's no cure for IC, but many treatments offer some relief, either singly or in combination. Figuring out what works can be hit-or-miss; there's no way to predict who will respond best to which treatment. Fortunately, increasing awareness and greater understanding of this complex disorder are helping to speed diagnosis and encourage research. In March 2011, the American Urological Association (AUA) issued its first set of guidelines for the diagnosis and management of interstitial cystitis/painful bladder syndrome. (A summary was published in the June 2011 Journal of Urology; the complete guidelines are available here: www.health.harvard.edu/ic_guidelines.) Also, the Agency for Healthcare Research and Quality (a federal research group that reviews what does and doesn't work in health care) is preparing a report on the effectiveness of treatments for chronic pelvic pain in women, including IC; the final report is expected in late 2011, but a draft is available here: www.health.harvard.edu/ic_report.
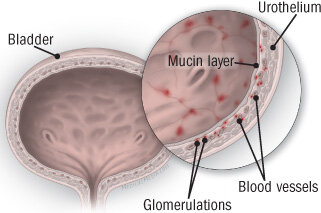
A defect in the layer of mucus (mucin layer) that protects the cells lining the bladder (the urothelium) may permit toxic substances from urine to seep through and inflame tissues. Irritated blood vessels produce tiny areas of bleeding in the bladder lining called glomerulations. Most people with interstitial cystitis have glomerulations.
Possible causes
No one knows the exact cause of IC; more than one mechanism is probably involved. Biopsies of the bladder wall in people with IC indicate various abnormalities, but it's not clear whether these are the cause of the condition or the result of some other underlying process. Some research has focused on defects in the glycosaminoglycan (GAG) layer, part of the layer of mucus that lines and protects the bladder. Defects in the GAG layer may allow toxins in the urine to leak through and damage underlying nerve and muscle tissues; this in turn may trigger pain and hypersensitivity.
Another line of research centers on antiproliferative factor (APF), a substance that's found only in the urine of people with IC. APF appears to block the normal growth of cells that line the bladder and may hinder the healing process that follows any damage or irritation to bladder tissues. Scientists seeking a diagnostic test for IC are considering APF as a possible
biomarker.
There are several other theories about the cause of IC. It may be an infection with an unknown agent, such as a virus. Or it may be an autoimmune disorder set in motion by a bladder infection. It's possible that mast cells normally involved in allergic responses are releasing histamine into the bladder. Another idea is that sensory nerves in the bladder somehow "turn on" and spur the release of substances that contribute to symptoms. Because interstitial cystitis is mainly a woman's disease, many researchers think that hormones play a role.
Variable symptoms
The onset of IC is usually gradual, with bladder pain and urinary urgency and frequency developing over a period of months. The course of the disorder and its symptoms can vary greatly from woman to woman and even in the same woman. Symptoms may change from day to day or week to week, or they may remain constant for months or years and then go away, only to return several months later. Pain ranges from dull and achy to acute and stabbing; discomfort while urinating fluctuates from mild stinging to burning. But virtually everyone with IC has pain associated with bladder filling and emptying. Some women with IC have a constant need to urinate, because urinating helps relieve the pain.
In women who also have chronic abdominal or pelvic pain from other causes, such as irritable bowel syndrome or endometriosis, IC may flare up when those symptoms are at their worst. Sexual intercourse can trigger pain lasting several days, and symptoms may worsen with menstruation. On the other hand, some women experience complete relief during the second and third trimesters of pregnancy. Some find that their symptoms are worse after consuming certain foods or drinks, including strawberries, oranges, tomatoes, chocolate, spices, caffeine, alcohol, and beverages that acidify the urine, such as cranberry juice.
Diagnosis of exclusion
IC is not a urinary tract infection, and it can't be identified by a simple urinalysis or urine culture. Rather, it's a diagnosis of exclusion, which means that it's diagnosed only after a number of other conditions have been ruled out. A clinician ? usually a urologist or a gynecologist ? will first take a thorough history, then conduct a physical exam (including a pelvic exam, if it's not too uncomfortable) and perform tests for infection, bladder stones, bladder cancer, kidney disease, multiple sclerosis, endometriosis, sexually transmitted diseases, and other disorders. The AUA guidelines also recommend an early assessment of pain, urinary frequency, and urine volume, to help evaluate the effectiveness of later treatments.
If a diagnosis is uncertain or there are symptoms (such as blood in the urine) that suggest other problems, the next step is usually cystoscopy, which involves inserting a fiber-optic tube through the urethra to look at the bladder wall. During the procedure, a tissue sample may be taken to rule out bladder cancer. Some clinicians favor hydrodistention under local or regional anesthesia, which involves filling the bladder during cystoscopy with a liquid that stretches it, providing a closer view of the bladder wall. However, AUA guidelines do not recommend hydrodistention for either diagnosis or treatment. In people with IC, glomerulations ? tiny pinpoint spots of blood ? are usually visible on the bladder wall during cystoscopy with hydrodistention, but these lesions are often seen within the normal bladder as well.
One finding from cystoscopy that can help in making an IC diagnosis is the presence of reddened patches or lesions called Hunner's ulcers, which can stiffen tissue and cause reduced bladder capacity. However, Hunner's ulcers, which occur in 10% to 15% of cases, aren't required to make an IC diagnosis.
The potassium sensitivity test, which involves instilling potassium chloride into the bladder to see if it triggers pain, has been proposed for use in diagnosing IC, but it's not conclusive and the AUA does not recommend it for routine use.
Managing IC
There's little consensus on the best way to treat IC, but treatment generally starts with conservative measures and proceeds to more invasive ones if symptoms don't improve. Usually a combination of approaches is needed, including
these:
Psychosocial support. Chronic pain can be an isolating experience, so it may help to be in touch with others who feel your pain and understand what you're going through. Local pain support groups or national support groups like the Interstitial Cystitis Association (see "Selected resources") can serve that purpose. Learning as much as you can about
IC may also give you a greater sense of control over your condition. Chronic pain can cause depression, so don't hesitate to consult a mental health professional if you're feeling overwhelmed. (Support groups can usually refer you to counselors.) You may also want to talk to someone who specializes in stress reduction techniques, such as guided imagery, which was shown in one controlled study to improve IC patients' response to therapy. Some people say
they've been helped by biofeedback, which trains people to use their minds to control physiological processes, such as muscle tension, that may be contributing to symptoms.
Behavior changes. Avoid anything that appears to cause flare-ups, whether that's a certain kind of exercise, sexual activity, constipation, tight clothing, or a specific food. (Because high-acid foods seem to cause flare-ups, some clinicians suggest taking an antacid with meals.) Expanding your bladder capacity is also important (constantly succumbing to the
urge to go all the time can shrink bladder capacity). For example, if you're urinating every 30 minutes, try holding off for 45 minutes; if you manage that for a week, increase the interval to 60 minutes the second week, and so forth.
Medications. Various medications may help relieve pain and reduce inflammation. (See "Medications for the treatment of interstitial cystitis.") Some are taken orally; others are bladder instillations ? drugs that are introduced into the bladder by catheter and held for a few seconds up to 10 or 15 minutes. Instillation usually takes place in a clinician's office, although in some cases, these drugs can be self-administered at home.
| Medications for | the treatment of interstitial cystitis |
| Treatment | Comment |
| Oral drugs | |
| Tricyclic antidepressants | Taken at low doses, tricyclic antidepressants relax the bladder and hinder the release of neurochemicals that can cause bladder pain and inflammation. They may also improve sleep. Amitriptyline (Elavil) is the medication most commonly prescribed for interstitial cystitis. Side effects include sleepiness, dry mouth, and weight gain. |
| Pentosan polysulfate sodium (Elmiron) | The only oral medication approved by the FDA specifically for the treatment of IC, Elmiron is thought to help repair defects in the bladder lining. It can take several months to reduce pain and urinary frequency, and the effect may be modest. Serious side effects are rare. If Elmiron doesn't work in six months, stop taking it. |
| Antihistamines | to block mast cells' release of histamine in the bladder. It helps in relieving pain, urinary frequency, and (because it's sedating) nighttime urination. Some clinicians recommend cimetidine (Tagamet) and ranitidine (Zantac), which are a different type of antihistamine, but there's little evidence to support their use. |
| Painkillers | Nonsteroidal anti-inflammatory drugs (aspirin, ibuprofen, naproxen sodium) and acetaminophen can help relieve mild to moderate pain. Opioid analgesics, such as oxycodone or hydrocodone combined with acetaminophen, may be used for severe pain when other therapies haven't worked, but they can be addictive. |
| Cyclosporine A | In early studies, this immunosuppressant drug helped relieve symptoms, but its use is limited by serious side effects ? including uncontrollable trembling, muscle or joint pain, and enlarged gums. |
| Bladder instillations | |
| Dimethyl sulfoxide (DMSO) | DMSO instilled in the bladder was FDA-approved for the treatment of IC in the 1970s. It helps relax the bladder and alleviate pain. Treatment involves weekly instillations for six to eight weeks and then every two weeks for three or more months. |
| Heparin and lidocaine | Some clinicians combine one or both of these drugs with Elmiron (as a bladder instillation) and other medications in "rescue instillations" administered to quickly reduce pain and inflammation and help restore the mucus in the bladder. |
Specialized physical therapy. Working with a physical therapist trained in pelvic soft tissue manipulation and rehabilitation may help to release scars and other sources of pelvic pain. Exercises that relax the pelvic floor are okay, but the AUA recommends that people with IC avoid exercises that strengthen pelvic floor muscles (Kegels).
Additional options. If standard treatments don't work, your clinician may suggest a trial of an implantable device called InterStim, which stimulates the sacral nerve in the lower back and may help alleviate urinary urgency and frequency in some women. If the device helps, it can be permanently implanted. Researchers are also studying the instillation of botulinum toxin into the bladder, but so far, the side effects and complications have been too serious to recommend its general use.
What doesn't work. The AUA found no evidence that the following therapies help relieve IC symptoms, and some evidence they may be harmful: long-term oral antibiotics, bladder instillation of bacillus Calmette-Guerin (BCG), and bladder instillation of resiniferatoxin (RTX).
Dr. Kathy Niknejad, Director of Surgical Specialties at Harvard Vanguard Medical Associates in Boston and instructor in surgery at Harvard Medical School, helped prepare this article.
Selected resources
American Urological Association Foundation
800-828-7866 (toll-free)
www.urologyhealth.org
Interstitial Cystitis Association
800-435-7422 (toll-free)
www.ichelp.org
Interstitial Cystitis Network
707-538-9442
www.ic-network.com
