David Baxter PhD
Late Founder
Treatment Resistant Depression: Options, Strategies, and More
by Morgan Meissner, MS, PsychCentral.comApril 1, 2021
Depression that doesn’t respond well to antidepressants is known as treatment-resistant depression.
About half of people experiencing depression symptoms may see a slight or no improvement when they take antidepressants. This leaves lingering symptoms that can strain your mental, emotional, and physical well-being.
However, there are steps you can take to effectively manage symptoms of depression.
What is treatment-resistant depression?
Experts say depression is treatment-resistant when your symptoms haven’t improved after you’ve tried two antidepressants. You must have taken them at the optimal dose for an appropriate amount of time to see an effect, usually about 4 to 6 weeks.If a healthcare professional has prescribed you two or more antidepressants and your depression symptoms persist, speak with a psychiatrist.
If you started your medication regimen with a psychiatrist or psychiatric nurse practitioner, ask them about the possibility of trying different solutions.
What to expect with a psychiatrist
A psychiatrist may begin asking questions to learn more about you. They may be particularly interested in finding out if you:- also have an anxiety or personality disorder
- smoke or use recreational drugs
- have other chronic, nonpsychiatric conditions, such as autoimmune diseases
To get a more complete picture of your health, the psychiatrist may also order blood work, such as:
- a complete blood count
- liver and kidney function tests
- lipid and glucose tests
- a thyroid test
These questions can also help determine whether the treatment resistance you’re experiencing is due to an undiagnosed, underlying condition.
For example, bipolar disorder is common among people experiencing treatment-resistant depression.
Medication strategies
You still have several options when it comes to medication for treatment-resistant depression.Antidepressants
Even if you’ve experienced resistance to antidepressants so far, they might still work for you.Your healthcare professional may try optimizing your current treatment by giving it more time to work or increasing the dose.
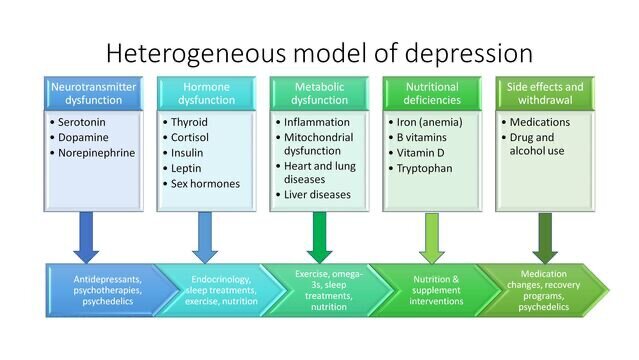
Different classes of antidepressants work in different ways, so your psychiatrist may also consider switching you to a different class of antidepressant.
Some common classes of antidepressant include:
- selective serotonin reuptake inhibitors (SSRIs)
- dual serotonin and norepinephrine reuptake inhibitors (SNRIs)
- tricyclic antidepressants (TCAs)
- monoamine oxidase inhibitors (MAOIs)
People who don’t respond to an SSRI may experience improved symptoms once they switch to a TCA, MAOI, or certain SNRIs, according to research.
Adjuvant treatments
Your doctor may also try adding another medication alongside your antidepressant to boost effectiveness. Healthcare professionals call this augmentation or adjuvant treatment.Some common adjuvants include:
- lithium
- thyroid hormone (T3)
- a second-generation antipsychotic, such as quetiapine, aripiprazole, olanzapine, or risperidone
- benzodiazepines or hydroxyzine, for people with anxiety
- a hypnotic, such as zolpidem or zopiclone, if you have trouble sleeping
Ketamine
In recent years, the drug ketamine has emerged as a potential option for treatment-resistant depression.Healthcare professionals originally used it as an anesthetic. However, new research has found that ketamine acts as a pain reliever and sedative at lower doses and exerts multiple effects on the parts of the brain associated with depression.
One systematic review of studies showed that it is generally safe for adults and that you may experience relief from depression symptoms as soon as 4 hours after using it.However, researchers know less about its effects in older people, children, and teenagers. More research is needed.
Research has shown that ketamine infusions are effective, but the drug is also available as a nasal spray.
Because the use of ketamine to treat depression symptoms is so new, there isn’t a standard protocol for how or when you should use it.
Generally, though, ketamine is reserved for people experiencing severe symptoms of treatment-resistant depression who need immediate relief, such as those at risk of suicide.
Therapy
Getting psychological counseling can help address the many ways depression symptoms affect your life, including your emotional, social, and physical health.People may call this psychotherapy, counseling, or talk therapy.
The goal of counseling is to discover the core issues underlying your symptoms and equip you with the tools to improve your sense of well-being and relieve feelings of distress.
Counseling can help you with decision-making skills, maintaining healthy relationships, stress management and coping techniques, and developing a healthy self-esteem.
Experts say the goals of psychotherapy or counseling are to:
- equip you with the tools to recognize when your symptoms are getting worse
- help you develop coping strategies for stressful situations
- provide psychological support for the symptoms of depression
- provide education about your condition
- help you stick with treatment recommendations
- manage other psychiatric conditions, such as anxiety or substance use disorder
What to try if therapy isn’t working
Counseling with a support therapist who listens well and provides occasional unstructured validation or advice does not tend to help people experiencing symptoms of depression.However, some specific psychotherapy techniques may be effective.
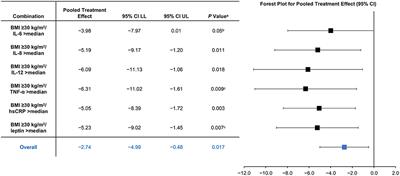
These may be even more beneficial if you receive them at the same time as you take antidepressant medications.
Research suggests that combining psychotherapy and antidepressant treatment improves or resolves symptoms in people experiencing treatment-resistant depression better than taking antidepressants independently.
According to the American Psychological Association (APA), most people experiencing treatment-resistant depression benefit from a combination of medication and psychotherapy.
Cognitive behavioral therapy
Cognitive behavioral therapy (CBT) is a form of psychotherapy that focuses on changing your mental and behavioral responses to stress.CBT is powerful because it also helps you respond to factors that contribute to depression. It may help you change negative thought patterns and engage in meaningful activities or behaviors.
This type of therapy empowers you to act as your own therapist so you can continue helping yourself over the long term.
One study looked at the effects of combining CBT and antidepressant medications. Those who received both were more than 3 times as likely to show long-term improvements in depression symptoms as those who took just antidepressants.
Even if you stop taking medication for depression symptoms, the skills you learned in CBT continue to help you throughout life.
Brain stimulation
Doctors reserve brain stimulation procedures as a last resort for people who have not responded well to multiple antidepressants or therapy.If you decide to try this treatment, a doctor will stimulate parts of your brain with electricity.
Electroconvulsive therapy (ECT) is the type of brain stimulation researchers have studied most. Healthcare professionals have used it since the early 1900s to treat mental health conditions.
Although portrayals of ECT in pop culture have often been negative, studies suggest that it can provide relief for many people who don’t respond to antidepressants.
ECT is also very safe in its modern form — an important point to consider if you’re wondering whether you should get it.
The APA generally recommends that doctors reserve ECT for people experiencing severe treatment-resistant depression, such as those who are experiencing suicidal thoughts or also experiencing psychosis.
If ECT doesn’t work to resolve symptoms, your doctor may recommend trying other brain stimulation techniques, such as:
- repetitive transcranial magnetic stimulation (rTMS)
- vagus nerve stimulation (VNS)
- deep brain stimulation
Living with treatment-resistant depression
There are many small steps you can take to help manage your symptoms of depression.Stick to your treatment plan
Even if you feel better, it’s advisable to keep taking your medications as prescribed and continue going to therapy. Depression symptoms could return if you stop treatment.If you have concerns about your medications, such as side effects that you don’t like, your psychiatrist may have other options.
Stress management techniques
Therapy can help you develop skills to cope with stress in a healthy, productive way.It can also help you manage particular factors related to depression, such as negative thought patterns or lack of enjoyment or motivation.
Self-care helps
Research suggests that people who eat a diet rich in fruits and vegetables are less likely to experience depression symptoms. It also recommends physical activity as a complement to antidepressant treatment.If you drink alcohol, smoke, or take recreational drugs, consider quitting. This may reduce symptoms of depression.
If you feel you need support for a substance use disorder, your healthcare professional may help.