Understanding Depression
Medscape Psychiatry and Mental Health
October 10, 2014
The Symptoms and Causes of Depression
What is depression? What causes it? These are common questions that patients ask me every day in my mental health clinic. However, the majority of patients with depression first present to their primary care physician. Do they know how to respond to these questions if asked by a patient?
Some patients may erroneously attribute their depression to personal weakness, or lack of faith or will. This stigma can be a barrier that keeps people from seeking help. It also makes those who suffer from depression feel even worse. Many patients who commit suicide visit a doctor in the week leading up to their death. Therefore, it is vitally important that all medical professionals understand the disease of depression, how to identify its signs and symptoms, and how to best educate their patients.
What Is Depression?
Depression is a feeling, and every person has a unique experience and description of the disease. It is important to feel comfortable educating your patients about depression, because your knowledge and care can give them hope and decrease the stigma associated with depression.
I start by explaining the following: Sometimes we feel "down" or "blue," and these feelings resolve after a few hours or days. These ups and downs of life are normal and should be expected. However, when the feeling of sadness lasts for more than 2 weeks, it is time to seek help. If your patient expresses that they have been depressed, reassure them that they are in the right place and you are here to help them. Empathy, concern, and a supportive environment can lift a large burden and is extremely therapeutic.
In many cases, patients will not come right out and say "I'm depressed." However, depression is often accompanied by other symptoms and may be the actual problem the patient presents with. Therefore, it is important that you know the signs and symptoms of depression so that you can identify them.
For example, people who are depressed can have trouble falling and staying asleep?or conversely, they will find they want to sleep all the time. Interest in things commonly enjoyed can disappear. Feelings of guilt and hopelessness can be intense and constant. Concentration is often impaired, and appetite can be minimal or, conversely, voracious. Time is spent staring into space or sitting around purposelessly. If you do not screen for these symptoms or discuss them with your patients, you could very well miss a patient suffering from depression. The American Psychiatric Association Provides a screening tool for depression that I encourage you to use.
It can be difficult to discuss the dangers of depression. Some providers fear that discussing suicide could make their patient worse or more likely to harm themselves. However, this is not the case. It is extremely important to discuss the dangers of depression so that patients know when they need to immediately seek further assistance and a higher level of care.
I discuss the following with my patients who are suffering from depression: The most severe and worrisome symptoms are thoughts about being better off dead, or harming or killing oneself or others. Depression is dangerous when it distorts thinking, judgment, and decision-making. The disease of depression can make it hard to remember the last time you felt "normal" and hard to believe you will ever feel "normal" again.
It can be hard to believe someone we have known as a happy, well-adjusted, and successful friend, neighbor, family member, or colleague would want to kill themselves. However, depression is extremely powerful, and sometimes suicide will seem like the only option.
Without this information, patients can feel lost or, worse, defeated if their symptoms progress. It is of utmost importance to educate your patients to get help right away if their mood worsens or if they have any of these additional symptoms. There is no reason for them to wait to seek help until they get to the point of thinking about harming themselves. If their mood is not improving or you feel uncomfortable managing their depression, assist them with making an appointment with a psychiatrist as soon as possible. If your patient had blurry vision, would you wait until they were blind before recommending that they see a specialist?
It is important to provide crisis numbers, including the national suicide hotline (1-800-273-8255), which is available 24/7. PCPs should advise their patients that if they are feeling dangerous to themselves, they should not wait to see a psychiatrist in the community; they should go to the nearest emergency department or call 911.
What Causes Depression
We know that some people are genetically predisposed to have a higher chance of episodes of depression throughout their lifetime. Educate your patients that if their parents or siblings have experienced depression, they are much more likely to as well. Understanding that they are at higher risk is important. Just as those with a family history of heart disease or cancer should be more diligently screened, the same is true for those with a family history of depression. Overall, however, a history of previous episodes of depression is the best predictor of future episodes.
The other area depression comes from is our environment. Stressors and triggers at home and work and memories can all negatively affect our patients' thoughts. I educate my patients about the following: Negative thoughts affect not only mood and feelings, but also behavior and biology (Figure 1).
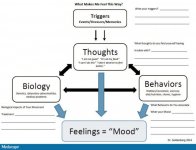
Figure 1.
Contributors to depression.
For example, depression can lead to self-isolation, poor diet, and limited exercise. All of these factors negatively affect biology. We know that the brain and its neurotransmitters change during an episode of depression (Figure 2).
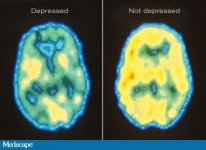
Figure 2.
Neuroimaging of depressed vs nondepressed brain.
Depression negatively affects behavior by decreasing engagement in recreational activities and making chores and hygiene more likely to be deferred. Not being able to keep up with responsibilities at work and at home can lead to additional negative thoughts, including "being a failure." Ever-increasingly negative thoughts, biology, and behavior all then enhance the feeling of depression. It is truly a vicious cycle. What starts as something minimal can quickly snowball into severe and debilitating depression that negatively affects the biological, psychological, and social aspects of our patients' lives.
The reason why it is so important for primary care physicians to understand the causes of depression, and to educate patients about them, is because these areas serve as targets of treatment. A thorough plan is multifaceted and addresses all of these areas.
What Else Do We Know About Depression?
We know that some people are at higher risk for depression than others. We know that depression can negatively affect all areas of a person's life. We know that feelings of hopelessness and distorted thoughts and judgment can lead to self-harm and suicide. We know that as for any disease, the symptoms and causes of depression can serve as the aim of our research and our treatments.
Furthermore, like most diseases that go untreated, depression negatively affects quality of life and has complications, the most serious of which is suicide. This is why it is so important that we decrease the negative stigma and encourage those suffering from depression to get help immediately.
We have all the tools needed to provide an empathetic and supportive environment to begin the process of recovery with our patients. If anyone you know is suffering from depression, please assist them in obtaining treatment right away.
Medscape Psychiatry and Mental Health
October 10, 2014
The Symptoms and Causes of Depression
What is depression? What causes it? These are common questions that patients ask me every day in my mental health clinic. However, the majority of patients with depression first present to their primary care physician. Do they know how to respond to these questions if asked by a patient?
Some patients may erroneously attribute their depression to personal weakness, or lack of faith or will. This stigma can be a barrier that keeps people from seeking help. It also makes those who suffer from depression feel even worse. Many patients who commit suicide visit a doctor in the week leading up to their death. Therefore, it is vitally important that all medical professionals understand the disease of depression, how to identify its signs and symptoms, and how to best educate their patients.
What Is Depression?
Depression is a feeling, and every person has a unique experience and description of the disease. It is important to feel comfortable educating your patients about depression, because your knowledge and care can give them hope and decrease the stigma associated with depression.
I start by explaining the following: Sometimes we feel "down" or "blue," and these feelings resolve after a few hours or days. These ups and downs of life are normal and should be expected. However, when the feeling of sadness lasts for more than 2 weeks, it is time to seek help. If your patient expresses that they have been depressed, reassure them that they are in the right place and you are here to help them. Empathy, concern, and a supportive environment can lift a large burden and is extremely therapeutic.
In many cases, patients will not come right out and say "I'm depressed." However, depression is often accompanied by other symptoms and may be the actual problem the patient presents with. Therefore, it is important that you know the signs and symptoms of depression so that you can identify them.
For example, people who are depressed can have trouble falling and staying asleep?or conversely, they will find they want to sleep all the time. Interest in things commonly enjoyed can disappear. Feelings of guilt and hopelessness can be intense and constant. Concentration is often impaired, and appetite can be minimal or, conversely, voracious. Time is spent staring into space or sitting around purposelessly. If you do not screen for these symptoms or discuss them with your patients, you could very well miss a patient suffering from depression. The American Psychiatric Association Provides a screening tool for depression that I encourage you to use.
It can be difficult to discuss the dangers of depression. Some providers fear that discussing suicide could make their patient worse or more likely to harm themselves. However, this is not the case. It is extremely important to discuss the dangers of depression so that patients know when they need to immediately seek further assistance and a higher level of care.
I discuss the following with my patients who are suffering from depression: The most severe and worrisome symptoms are thoughts about being better off dead, or harming or killing oneself or others. Depression is dangerous when it distorts thinking, judgment, and decision-making. The disease of depression can make it hard to remember the last time you felt "normal" and hard to believe you will ever feel "normal" again.
It can be hard to believe someone we have known as a happy, well-adjusted, and successful friend, neighbor, family member, or colleague would want to kill themselves. However, depression is extremely powerful, and sometimes suicide will seem like the only option.
Without this information, patients can feel lost or, worse, defeated if their symptoms progress. It is of utmost importance to educate your patients to get help right away if their mood worsens or if they have any of these additional symptoms. There is no reason for them to wait to seek help until they get to the point of thinking about harming themselves. If their mood is not improving or you feel uncomfortable managing their depression, assist them with making an appointment with a psychiatrist as soon as possible. If your patient had blurry vision, would you wait until they were blind before recommending that they see a specialist?
It is important to provide crisis numbers, including the national suicide hotline (1-800-273-8255), which is available 24/7. PCPs should advise their patients that if they are feeling dangerous to themselves, they should not wait to see a psychiatrist in the community; they should go to the nearest emergency department or call 911.
What Causes Depression
We know that some people are genetically predisposed to have a higher chance of episodes of depression throughout their lifetime. Educate your patients that if their parents or siblings have experienced depression, they are much more likely to as well. Understanding that they are at higher risk is important. Just as those with a family history of heart disease or cancer should be more diligently screened, the same is true for those with a family history of depression. Overall, however, a history of previous episodes of depression is the best predictor of future episodes.
The other area depression comes from is our environment. Stressors and triggers at home and work and memories can all negatively affect our patients' thoughts. I educate my patients about the following: Negative thoughts affect not only mood and feelings, but also behavior and biology (Figure 1).
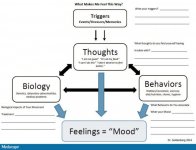
Figure 1.
Contributors to depression.
For example, depression can lead to self-isolation, poor diet, and limited exercise. All of these factors negatively affect biology. We know that the brain and its neurotransmitters change during an episode of depression (Figure 2).
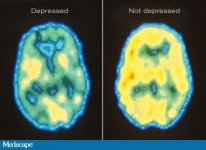
Figure 2.
Neuroimaging of depressed vs nondepressed brain.
Depression negatively affects behavior by decreasing engagement in recreational activities and making chores and hygiene more likely to be deferred. Not being able to keep up with responsibilities at work and at home can lead to additional negative thoughts, including "being a failure." Ever-increasingly negative thoughts, biology, and behavior all then enhance the feeling of depression. It is truly a vicious cycle. What starts as something minimal can quickly snowball into severe and debilitating depression that negatively affects the biological, psychological, and social aspects of our patients' lives.
The reason why it is so important for primary care physicians to understand the causes of depression, and to educate patients about them, is because these areas serve as targets of treatment. A thorough plan is multifaceted and addresses all of these areas.
What Else Do We Know About Depression?
We know that some people are at higher risk for depression than others. We know that depression can negatively affect all areas of a person's life. We know that feelings of hopelessness and distorted thoughts and judgment can lead to self-harm and suicide. We know that as for any disease, the symptoms and causes of depression can serve as the aim of our research and our treatments.
Furthermore, like most diseases that go untreated, depression negatively affects quality of life and has complications, the most serious of which is suicide. This is why it is so important that we decrease the negative stigma and encourage those suffering from depression to get help immediately.
We have all the tools needed to provide an empathetic and supportive environment to begin the process of recovery with our patients. If anyone you know is suffering from depression, please assist them in obtaining treatment right away.
