Hypervigilance and How it Wires the Pain Response Deeper - Pathways
Let’s look at what hypervigilance is, how it can increase the pain response and what can be done about it.
 www.pathways.health
www.pathways.health
January 16, 2020
Let’s look at what hypervigilance is, how it can increase the pain response and what can be done about it.
Acute pain is an alarm system, telling you that something is wrong. Acute pain lets you know that you have an injury or that there is a threat in your environment, and you need to pay attention! So, it’s natural that when you feel pain, you would be very aware of it.
However chronic pain, meaning pain which lasts longer than 3-6 months, doesn’t signal damage or injury. Like a faulty alarm system, chronic pain is your nervous system sending out too many or amplified pain messages. That means you are feeling pain despite it serving no protective purpose! Therefore, focusing too much attention on chronic pain is unhelpful. In fact, it can actually make your chronic pain worse and hardwire your pain response even deeper!
What is hypervigilance?
When you are constantly aware of your pain, considering it in every action throughout your day, this is known as being hypervigilant. It’s as though your senses are on overdrive, constantly on the lookout for perceived ‘threats’ which could worsen your pain.This study defines hypervigilance as, “an enhanced state of sensory sensitivity accompanied by an exaggerated scan or search for threatening information.”
How does hypervigilance wire the pain response deeper?
Our brain is neuroplastic, which means that it changes as it learns from what is happening in our environment and what we experience throughout our lives. Chronic pain literally changes our neural pathways, making them more sensitive, essentially teaching our brains and nervous systems to continue sending out these pain messages. This is also known as central sensitization, simply meaning that our nervous system is in overdrive.Constant awareness and fear of what is going to worsen your pain is reinforcing to your brain that these situations ‘should’ cause pain, wiring these neural pathways even more deeply. Hypervigilance is basically letting your brain and nervous system know that these pain responses are correct rather than faulty and that it should continue producing them.
For example, if your brain is sending pain messages when you walk across the room, you may become extremely aware of this. You start expecting pain when you walk across the room and perhaps even avoiding the action. When this happens, you’re telling and reinforcing to your brain that, “yes walking across the room causes pain”. Just like we learn any new skill or habit, the pain response can start turning on automatically without any physical stimuli or damage to our body being present.
This study found that patients who were hypervigilant about their pain were more sensitive to pain, explaining that, “The hypervigilance model of pain perception states that chronic pain patients have a heightened sensitivity to pain (e.g. low threshold and tolerance) because of increased attention to external stimulation and a preoccupation with pain sensations.”
Our brain has neurons known as mirror neurons, which start to send out signals through your nervous system even when you are just thinking about moving or when you’re watching someone else move. When you think about walking across the room in our example, the same neurons are activated as when you are actually carrying out the action, as explained in this study. This means that even imagined movements can cause pain!
Focusing on pain in a certain area of your body or worrying about an action causing pain, can cause these mirror neurons to jump into action, making your pain worse! This study explains that paying attention to pain in a specific area of the body makes the pain itself more intense, as well as the emotional impact and distress that comes with it, explaining that, “Paying attention to nociceptive input renders it more painful.”
Hypervigilance can contribute to catastrophizing, meaning you are plagued by negative thoughts and expectations of your pain, sometimes even before pain has occurred. This can influence your behaviour and make you more likely to engage in maladaptive (unhelpful) behaviours as explained here. This state of anxiousness and worry can be very emotionally distressing, taking a toll on your mental health. This study explains that, “pain hypervigilance was positively associated with greater pain intensity, emotional distress, psychosocial disability and pain-related health care utilization.”
While you are so focused on detecting perceived threats, your system becomes overworked. Your senses are not designed to be on high alert for such long periods of time. Being focused on pain levels so much makes it harder for the patient to actually detect real threats in their environment, as explained here.
This focus on your pain, results in it being impossible to focus your full attention on other tasks. This can make it tough to function, to relax, to sleep, to enjoy pleasurable activities or to work as explained in this study.
When your body doesn’t get the rest it needs, this increases fatigue and contributes to chronic pain. Being on high alert all the time means that you are always tense and anxious, stuck in a constant state of ‘fight or flight’, which your body is not designed to cope with long-term. This prolonged stress state perpetuates the stress and pain cycle, worsening your pain.
Constantly being worried about what is going to make your pain worse can lead to avoidance of activity: this is also known as fear avoidance. As you start to avoid activity and movement, your body becomes deconditioned meaning that the muscles become weakened. This deconditioning then exacerbates your chronic pain when you do engage in any activity.
Fear avoidance also emphasises once again to the nervous system that it ‘should’ produce pain messages in reaction to these situations, increasing your pain levels. This avoidance of activity means that the patient’s level of functioning reduces, making them socially isolated and often unable to keep up with daily tasks.
How can hypervigilance be treated?
This all sounds worrying, but just as your brain can learn to produce chronic pain, it can also learn to stop producing those pain messages! Hypervigilance is a natural reaction to pain and certainly isn’t your fault. This article explains this aptly, “We have not evolved to ignore warning signals. To do nothing in the face of pain interruption is not only counter-cultural but it is also counter-biological.”However, hypervigilance is something you can change in order to reduce the impact pain has on your life. There are several therapies that can help with hypervigilance. You can access these through your doctor or specialist, seek them out privately or access them online through a chronic pain relief app like ours.
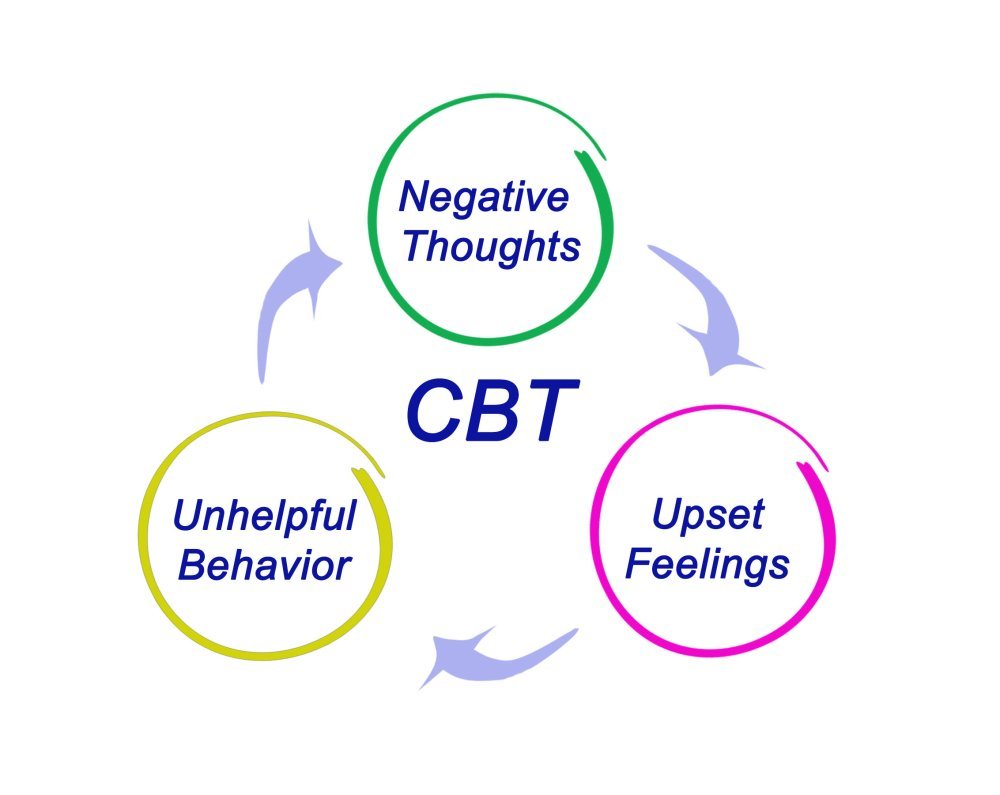
Cognitive Behavioural Therapy (CBT)
CBT is a talking based therapy which can help you to replace negative thoughts and their associated behaviours with positive, helpful thoughts and actions. CBT gives you the tools to cope with your pain in a healthier, more productive way.
CBT can reduce the pain itself as well as improving your quality of life and level of functioning. This study explains the effectiveness of “cognitive-behavioral interventions in improving pain coping skills and reducing pain, physical disability, and psychological disability.”

Acceptance and Commitment Therapy (ACT)
ACT focuses on helping you to accept your pain, to understand the cause of it and not allow negative thoughts to develop into negative behaviours. ACT can allow you to have greater control over your life, empowering you to face situations that you may have otherwise avoided through fear.
Graded Exposure Therapy (GET)
GET guides patients through facing situations that they avoid in a gradual way. GET introduces each movement over time in a step by step way, breaking the association between pain and that movement to retrain the brain. Over time the brain is given positive feedback, learning that the movement doesn’t need to be feared or cause pain.
GET can tackle fear avoidance, hyperligence and catazrophiszation effectively. This study found that, “graded exposure intervention led to reductions in pain hypervigilance, pain intensity, pain catastrophizing, and fear of pain, as well as improvements in daily functioning.”
Mindfulness
Learning to be mindful is about learning to be present in the moment, not worrying about the past or the future. These skills can be learnt through guided mindfulness meditations or mindfulness exercises and can be applied to your daily life at home.
Mindfulness can reduce stress, help you to reduce worry and anxiety, and enable you to redirect your focus to the task at hand rather than allowing your mind to wander.
A potential future treatment
Currently being trialled is Attentional Retraining for Chronic Pain Patients. This is a type of therapy which teaches patients to redirect their attention from their pain, teaching them to focus on more positive thoughts and behaviours. This treatment, if found to be successful, would be carried out at home, equipping patients with the tools to distract themselves from their pain and focus on productive tasks at hand. The clinical trial records explain that, “These techniques have been widely validated in anxious or addictive populations but have never been used to date in chronic pain patients.” The results will be released in January 2020 and could potentially provide a new approach to treatment of hypervigilance.Fundamentally, hypervigilance is a natural reaction to pain. While it isn’t a helpful reaction, it is possible to overcome hypervigilance in order to reduce your chronic pain, improve your quality of life and increase your level of functioning!
References
- Annals of Behavioural Medicine, Volume 48, Issue 1, Matthew S. Herbert, M.A., Burel R. Goodin, Ph.D.,Samuel T. Pero, IV, B.S., et al, (2014), “Pain hypervigilance is associated with greater clinical pain severity and enhanced experimental pain sensitivity among adults with symptomatic knee osteoarthritis”
- The Clinical Journal of Pain, Geert Crombez; Chris Eccleston ;Annelies Van den Broeck, et al, (2004), “Hypervigilance to Pain in Fibromyalgia: The Mediating Role of Pain Intensity and Catastrophic Thinking About Pain”
- PAIN, Volume 66, Issues 2–3, Pages 133-144, Ann J McDermid, Gary B Rollman, Glenn A McCain, (1996), “Generalized hypervigilance in fibromyalgia: evidence of perceptual amplification”
- PAIN, Volume 72, Issues 1–2, Pages 209-215, Chris Eccleston, Geert Crombez, Sarah Aldrich, CathyStannard (1997), “Attention and somatic awareness in chronic pain”
- Journal of Pain Research, Volume 11, Vossen CJ, Luijcks R, van Os J, Joosten EA, Lousberg R, (2017), “Does pain hypervigilance further impact the lack of habituation to pain in individuals with chronic pain? A cross-sectional pain ERP study”
- Journal of Neural Transmission, Th. Mulder, (2007), “Motor imagery and action observation: cognitive tools for rehabilitation”
- U.S. National Library of Medicine, Clinical Trials, (2019), “Attentional Re-training for Chronic Pain Patients (ABCD)“
- The Psychologist, Vol.24, pp.422-425, Christopher Eccleston, (2011), “A normal psychology of chronic pain”