Too Tired for More: How Best to Treat Multifactorial Fatigue
Fatigue: a very common physical complaint that often accompanies depressive disorders.
In this installment of Tales From The Clinic: The Art of Psychiatry, we review a very common physical complaint that often accompanies depressive disorders: fatigue. Its etiology, mental and physical, is difficult to disentangle and treatment remains elusive. In this article, Drs Khan and Ukrani walk us through therapeutic options and, most importantly, explain how to think about this ubiquitous presentation to best help our patients.
Case Study
“Ms Riley” is a 35-year-old woman who has received diagnoses of systemic lupus erythematosus (SLE) and recurrent major depression. She began coming to our clinic after the retirement of her former psychiatrist, whom she had been seeing for several years. Although treated with numerous antidepressants for her depression, she continues to have persistent symptoms—particularly fatigue—with remission difficult to obtain. Her previous psychiatrist prescribed aripiprazole to help with these persistent symptoms. She reached her best period of stability with a combination of aripiprazole, vilazodone, and buspirone.
She is married with 2 young children and had postpartum depression after both pregnancies. Although her marriage is stable overall, she and her husband had some strain regarding finances and the chronicity of her symptoms, which had previously led to hospitalizations for suicidal ideation. She is employed as an accountant, but her fatigue makes it difficult for her to stay on top of her work and meet deadlines. Her depression is relatively well controlled from the standpoint of mood, but she and her specialists have discussed whether her fatigue is related to lupus or is a residual symptom of depression.
Fatigue in Depression
Although we can often achieve response in patients with major depressive disorder (MDD), remission is a more difficult target, and many patients continue to have residual symptoms. Fatigue, which is ubiquitous across a variety of illnesses, is one of the most common residual symptoms of depression and overlaps with anhedonia, decreased energy, and other depressive dimensions. It can diminish performance at school and at work, disturb social and family relationships, and increase health care utilization. Patients with MDD and persistent symptoms of fatigue are substantially more likely to develop active depressive symptoms again despite continued treatment. Therefore, it is essential to recognize these symptoms and intervene as soon as possible.1,2
An article by Baldwin and Papakostas describes strategies to address fatigue, including the use of antidepressant medications that are less likely to induce or exacerbate fatigue and more likely to resolve it and the use of adjunctive treatments to target residual fatigue and sleepiness in patients with MDD specifically.3
The first approach entails avoiding medications with higher reported rates of fatigue or tiredness as an adverse effect (eg, tricyclic antidepressants, mirtazapine, duloxetine, and trazodone) in favor of those that are less sedating. Some options that may lead to better outcomes with fatigue include selective serotonin reuptake inhibitors (SSRIs), bupropion, alternate serotonin-norepinephrine reuptake inhibitors, and norepinephrine reuptake inhibitors like venlafaxine or reboxetine, agomelatine, tianeptine, and monoamine oxidase inhibitors. Although data are limited, there are some representative studies of fluoxetine, reboxetine (not available in the United States), and bupropion. In a study by Judge et al, fluoxetine showed greater efficacy than placebo in resolving retardation factor scores, including in older patients with depression.4 In a pooled analysis, bupropion was more effective than placebo and SSRIs in resolving hypersomnia and fatigue. In this same analysis, SSRIs did not separate from placebo with regards to hypersomnia but did appear more effective in resolving fatigue.
Finally, pharmacologic augmentation strategies may be used to treat residual fatigue. Bupropion is also a viable augmentation strategy. Masand et al demonstrated the effectiveness of stimulants in a small case series,5 and atomoxetine has also been shown to improve remission rates and reduce fatigue. Although the evidence for modafinil, specifically in hypersomnia and fatigue, has been mixed, it is more consistent regarding its improvement of overall depression.3,6
Fatigue in SLE [systemic lupus erythematosus]
SLE is an autoimmune disease that causes widespread inflammation and tissue damage in affected organs. Patients with SLE may experience fatigue, skin rashes, fevers, and pain or swelling of the joints. Some patients will have symptom flares interspersed with periods of remission, while others will have more persistent symptoms.7
Patients with SLE often report fatigue as a significant and debilitating symptom, but its etiology remains poorly understood due to its likely multifactorial nature. There have been conflicting findings about the link between disease activity and degree of fatigue, the dimensions of which include general, mental, and physical fatigue and reduced activity and motivation. All of these are elevated in patients with SLE.8 In a multivariate analysis, disease activity and damage and the presence of fibromyalgia significantly correlated with physical fatigue and were independent contributors.8 However, disease-related factors were not found to be significant predictors of mental fatigue. Investigators also found that 23% of patients had clinically significant depressive symptoms and that this depressed mood was associated with worse physical and mental fatigue. In the analysis, it was a stronger determinant of mental fatigue but correlated with both. Impaired sleep and low levels of exercise also contributed to increased fatigue.
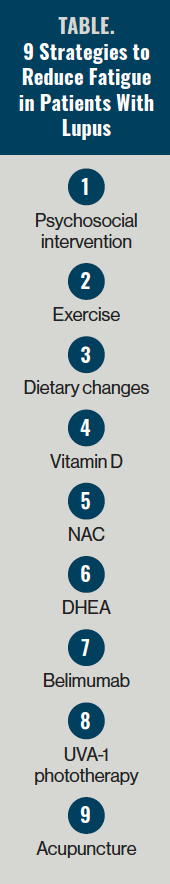
In a systematic review of the optimal management of fatigue in patients with SLE, Yuen and Cunningham identified 9 reduction strategies (Table).9 For psychosocial interventions, they found that nearly half of patients with SLE reported ongoing distress over time. There is an association between distress and fatigue, and thus patients may benefit from psychosocial interventions like cognitive behavioral therapy, psychoeducation, counseling, psychotherapy, and biofeedback to decrease disease interference with daily activities and improve interpersonal relationships, social support, self-efficacy, and stress-coping skills. Yuen and Cunningham reviewed several studies related to exercise, hypothesizing that because physical inactivity is associated with fatigue, increased activity would reduce fatigue. The exercise programs’ primary goals were to improve exercise tolerance, aerobic capacity, and perceived physical function, and to relieve fatigue. In addition, nearly half of adults with SLE are obese. Obesity is independently associated with impaired functional capacity and inflammation markers in patients with lupus. If patients lose weight, they may improve their functional capacity.10
Many SLE treatments can impact vitamin D metabolism and put patients with SLE at risk of vitamin D deficiency. However, the evidence for a correlation between vitamin D deficiency and fatigue is mixed. N-acetylcysteine (NAC), an amino acid precursor of glutathione, serves as an inhibitor of autoimmune inflammatory processes. Some data suggest that patients with SLE have low levels of glutathione and may then benefit from NAC supplements. In the studies reviewed by Yuen and Cunningham, doses of 2.4 g/day and 4.8 g/day led to significant improvement in fatigue, but the 4.8 g/day dose was not as well tolerated.9
Data also suggest that patients with SLE have lower mean serum levels of 5-dehydroepiandrosterone (DHEA), an androgen with immunomodulatory properties, which might be associated with increased fatigue. Belimumab is a monoclonal antibody that modulates B-lymphocyte stimulator protein and inhibits its activity. Patients with SLE have high stimulator protein levels and are correlated with changes in disease activity. Ultraviolet-AQ (UVA-1) phototherapy has emerged as a potential adjuvant therapy for SLE, while acupuncture is a treatment option for patients with fatigue-related pain who do not want to rely on medications to control it.
Yuen and Cunningham found weak evidence not meeting the minimal clinically important difference threshold in the various studies for psychosocial interventions, dietary changes, vitamin D supplementation, and acupuncture; no effect from DHEA; and weak to moderate effect in a small pilot randomized controlled trial with UVA-1 phototherapy. NAC was found to have moderate benefit in 1 small pilot study, which is promising. Aerobic exercise and belimumab appear to have the most substantial evidence for treatment efficacy for fatigue management in patients with SLE. Although the evidence for psychosocial interventions is weak, these interventions do lead to improvement in pain and distress reduction and thus may be beneficial. Yuen and Cunningham concluded that optimal management of fatigue for patients with SLE should start with lifestyle changes, including exercise and dietary modifications to help with weight loss and physical activity. Vitamin D supplementation should be considered when there is vitamin D hypovitaminosis. As NAC has few adverse effects and is relatively affordable, it may be considered with its early promising data. Belimumab has better evidence, but its high cost and adverse effects may limit its use. UVA-1 has some early encouraging data but safety concerns and exacerbation of SLE remain, so caution should be exercised. Lastly, acupuncture may benefit those with significant pain associated with their SLE and those who do not want to rely on medication.
Exploring Options
Fatigue remains a nonspecific symptom of numerous diseases and is likely multifactorial in etiology across this spectrum. In the case of our patient, her fatigue may arise as a residual symptom of her depression or as a symptom of her SLE. Further complicating this picture, her SLE may be contributing to her ongoing depressive symptoms, as nearly a quarter of all patients with SLE also report clinically significant depression symptoms. Although this Gordian Knot of etiology may be impossible to disentangle, another question arises: Does this matter?
On the one hand, as we can see in the review of treating fatigue across our patient’s illnesses, some common factors arise. Exercise can reduce both fatigue and depressive symptoms.11 Behavioral therapy and psychosocial interventions can be similarly beneficial, and acupuncture may result in a moderate reduction of depression, although the current quality of the evidence is very low.12
From a pharmacologic standpoint, some options for treating depression and/or the fatigue related to depression are bupropion, atomoxetine, modafinil, and psychostimulants. Additionally, there are 2 case reports of improved lupus-associated fatigue with modafinil.13 Although Mertz et al reported that the exact benefits of antidepressants on fatigue in SLE is are difficult to assess due to a lack of studies, there is “no reason to believe that those treatments would not be appropriate,” barring drug-drug interactions.14 Similarly, evidence for NAC is emerging in human and animal studies of SLE and depression.15
On the other hand, when etiology is unclear, clinicians may refer patients to other specialists rather than address the issue, either because they did not recognize it or because they think it is outside their scope of practice. Especially when mental health is involved, there is the risk for patients to experience diagnostic overshadowing, where physical illness symptoms are attributed to a mental illness16; the term treatment overshadowing has been proposed to describe possible treatment biases in actual treatment decisions. Our patient had experienced this previously, with the thought that her fatigue must have been due to her depression, or that a stimulant was “only” for attention-deficit/hyperactivity disorder and therefore would need to be prescribed by a psychiatrist.
Case Study Conclusion
In our clinic, we encounter many medically complex conditions with multifactorial symptoms that impact the daily life and functioning of patients like Ms Riley. Symptoms like fatigue can have far-reaching effects on quality of life, work and financial stability, family relationships, and self-image. In Ms Riley’s case, her fatigue and chronic symptoms strained her marriage, she struggled at work, she could not keep up with her children at home, and she often felt that she was placing too many house duties on her spouse. All of this led to a chronically negative self-image and the feeling of being too tired to do more.
With the belief that this fatigue was likely multifactorial, a stimulant was started. With titration of lisdexamfetamine, Ms Riley felt she was able to achieve a tenuous stability and took part in individual and couples’ therapy to improve her self-esteem, increase her feelings of being “good enough,” and work with her spouse on their relationship.
After several months, however, complications arose when she became pregnant again. She was worried about the potential effects of the medication on pregnancy and breastfeeding but also feared that discontinuing some of her medications could worsen her symptoms, make it difficult to function at work, or increase the risk of developing postpartum symptoms again. A discussion is worth a separate investigation into treating clinically complex patients through pregnancy, but we hope this case highlights the thoughtfulness needed to manage these complex patients and the reward for both patients and clinicians alike.
Dr Khan is medical director, associate program director of general psychiatry residency, and an assistant professor in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine in Houston, Texas. Dr Ukraniis a PGY-1 internal medicine resident at Mercy Fitzgerald Hospital.
References
1. Targum SD, Fava M. Fatigue as a residual symptom of depression. Innov Clin Neurosci. 2011;8(10):40-43.
2. Demyttenaere K, De Fruyt J, Stahl SM. The many faces of fatigue in major depressive disorder. Int J Neuropsychopharmacol. 2005;8(1):93-105.
3. Baldwin DS, Papakostas GI. Symptoms of fatigue and sleepiness in major depressive disorder. J Clin Psychiatry.2006;67(suppl 6):9-15.
4. Judge R, Plewes JM, Kumar V, Kopp JB. Changes in energy during treatment of depression: an analysis of fluoxetine in double-blind, placebo-controlled trials. J Clin Psychopharmacol. 2000;20(6):666-672.
5. Masand, PS, Anand VS, Tanquary JF. Psychostimulant augmentation of second generation antidepressants: a case series. Depress Anxiety. 1998;7(2):89-91.
6. Chang T, Fava M. The future of psychopharmacology of depression. J Clin Psychiatry. 2010;71(8):971-975.
7. Systemic Lupus Erythematosus (SLE). Centers for Disease Control and Prevention. July 5, 2022. Accessed January 25, 2023. Systemic lupuserythematosus (SLE)
8. Da Costa D, Dritsa M, Bernatsky S, et al. Dimensions of fatigue in systemic lupus erythematosus: relationship to disease status and behavioral and psychosocial factors. J Rheumatol. 2006;33(7):1282-1288.
9. Yuen HK, Cunningham MA. Optimal management of fatigue in patients with systemic lupus erythematosus: a systematic review. Ther Clin Risk Manag. 2014;10:775-786.
10. Oeser A, Chung CP, Asanuma Y, et al. Obesity is an independent contributor to functional capacity and inflammation in systemic lupus erythematosus. Arthritis Rheum. 2005;52(11):3651-3659.
11. Conn VS. Depressive symptom outcomes of physical activity interventions: meta-analysis findings. Ann Behav Med. 2010;39(2):128-138.
12. Smith CA, Armour M, Lee MS, et al. Acupuncture for depression. Cochrane Database Syst Rev. 2018;3(3):CD004046.
13. Korsten P, Piantoni S. Improvement of lupus-associated fatigue with modafinil: report of two cases. Lupus. 2021;30(6):1013-1016.
14. Mertz P, Schlencker A, Schneider M, et al. Towards a practical management of fatigue in systemic lupus erythematosus. Lupus Sci Med. 2020;7(1):e000441.
15. Giménez-Palomo A, Dodd SM, et. al. Exploring N-acetylcysteine in psychiatry. Psychiatric Times. 2020;37(8):48-51.
16. Jones S, Howard L, Thornicroft G. ‘Diagnostic overshadowing’: worse physical health care for people with mental illness. Acta Psychiatr Scand. 2008;118(3):169-171.

