MANAGING THE END OF THE ROAD FOR YOUR PETS: PALLIATIVE CARE FOR THE CANCER PATIENT 
by Sara Allstadt Frazier, DVM, Diplomate ACVIM (Oncology)
Approximately half of senior-aged dogs and one-third of cats will die of cancer, and thus it is likely that the general practitioner will have to manage patients with cancer. Regardless of the treatment options chosen, the patient’s comfort level is most important when managing cancer. The incidence of pain associated with cancer in humans is reported to be as high as 90%, and while such data is not available for dogs, some estimates suggest that roughly 50% of cancer-bearing dogs experience pain. In the author’s experience, tumors that most likely cause pain and discomfort include tumors of the bone, oral cavity, urogenital tract, head (particularly ocular and nasal tumors), and gastrointestinal tract, as well as those tumors that affect nerves or nerve roots. Additionally, tumors that become ulcerated also appear to cause significant discomfort. This is a brief review of palliative care options, most of which can be utilized in the general practice setting. The goal of palliative care is to achieve the best quality of life for patients and their families.
Assessment of Pain
Assessment of pain in veterinary patients can be a challenge and it is important to use a “team approach” to pain assessment in our patients. First, assess the patient and look at the patient’s interaction and behavior with its owners, with you, and with your staff. Is the patient guarding the affected area? Is the patient reluctant to move and interact? Is the patient’s attitude and interaction normal, based on past experience with that pet? Then, perform your physical exam and assess palpation-induced pain. Ask your team members who know the pet well for their thoughts on how the pet is doing. Then, quiz the owner on the day-to-day activity of the pet, the pet’s ability to ambulate well, the pet’s quality of sleep and appetite, and the pet’s participation in favorite activities.
Sometimes owners have a hard time seeing slow, day-to-day declines in their pets that may be more obvious to the veterinary team. One useful question to ask is, “What are your dog’s three favorite things?” Favorite activities may be greeting the owner at the door, eating, chasing a ball or other toy, or playing with the family. Ask if the pet is still active in these things. If not, then this is a sign that the patient’s quality of life may not be optimal.
Pain Management
Tumors that commonly cause pain include oral tumors, bone tumors, nerve sheath tumors (particularly those that affect the brachial plexus), nasal tumors, ocular tumors, urogenital tumors, pancreatic and gastrointestinal tumors, and ulcerated skin tumors. The author strongly recommends starting a pain management regimen as soon as tumors in these locations are diagnosed, as early intervention leads to better control of pain.
Generally, starting with a nonsteroidal anti-inflammatory drug (NSAID) is recommended. For tumors affecting bone, often an NSAID alone is not sufficient, and the addition of tramadol, gabapentin, and/or amantadine may be indicated. Bisphosphonates should also be considered in patients with osteolytic bone lesions, although further study is required to fully characterize the usefulness of this class of drug for pain management. The author has observed several patients who benefited significantly from treatment with this class of drugs; thus, it may be worthwhile trying a course in dogs with bone lesions.
In dogs with oral squamous cell carcinoma (OSCC), complete responses have been documented to piroxicam alone, and therefore this NSAID is recommended to manage this particular tumor. In cats with OSCC, meloxicam is recommended due to the poor pharmacokinetics of piroxicam in cats. Owners should be cautioned about the risk of nephrotoxicity with both of these drugs; however, given the short expected survival times in these cats, renal toxicity is often not the life-limiting factor. Additional pain medications are often required to alleviate bone pain. Many dogs and cats are successful in hiding their pain, and owners and veterinarians alike may be challenged to recognize the symptoms of pain in these patients.
Radiation Therapy
A palliative course of radiation therapy is often very useful for managing bone pain. For primary bone tumors such as osteosarcoma, approximately three out of four patients will experience some alleviation of pain in response to radiation therapy. Oral tumors commonly shrink with radiation therapy, and thus both pain relief and reduction of the physical mass may be achieved with this modality. Often, palliative courses of radiation therapy are administered once a week for a total of four weeks, although other courses may be recommended, depending on the tumor type and location. Round cell tumors such as histiocytic sarcoma or multiple myeloma commonly affect bone and typically respond very favorably to radiation.
Combination Therapy
Combination therapy is recommended in most cancer patients, as it is unlikely that any one drug will alleviate all pain associated with cancer. The author typically starts with an NSAID and tramadol, adding in gabapentin, Tylenol 3 or 4 (in dogs only), or amantadine as needed. Gabapentin and amantadine seem to be particularly useful to manage neuropathic pain. Caution should be used when combining drugs that affect the serotonergic system (tramadol, amantadine, amitriptyline, mirtazapine); it is recommended to not use more than two of these in combination.
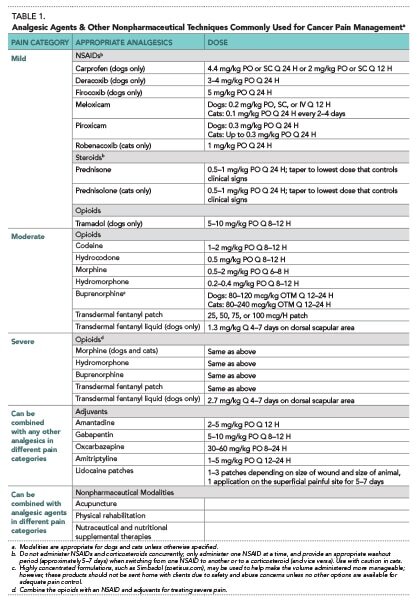
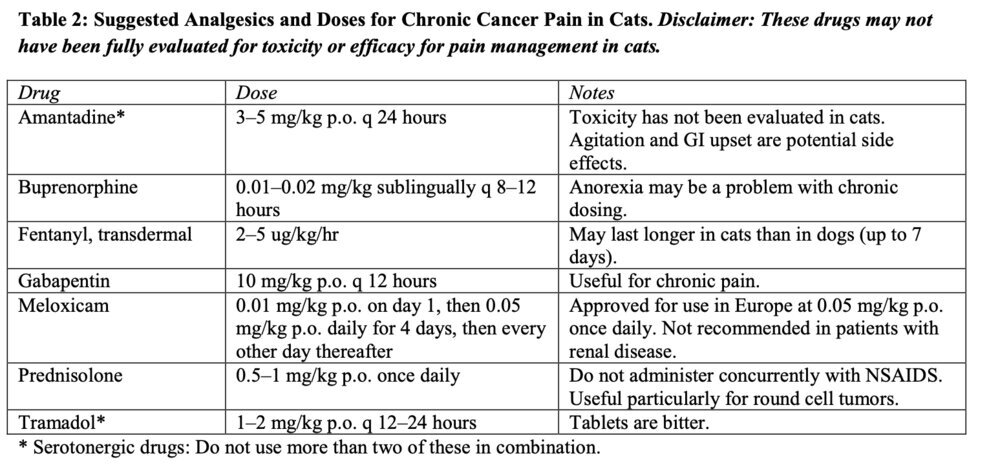
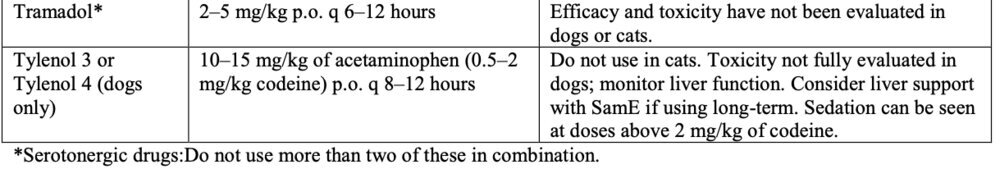
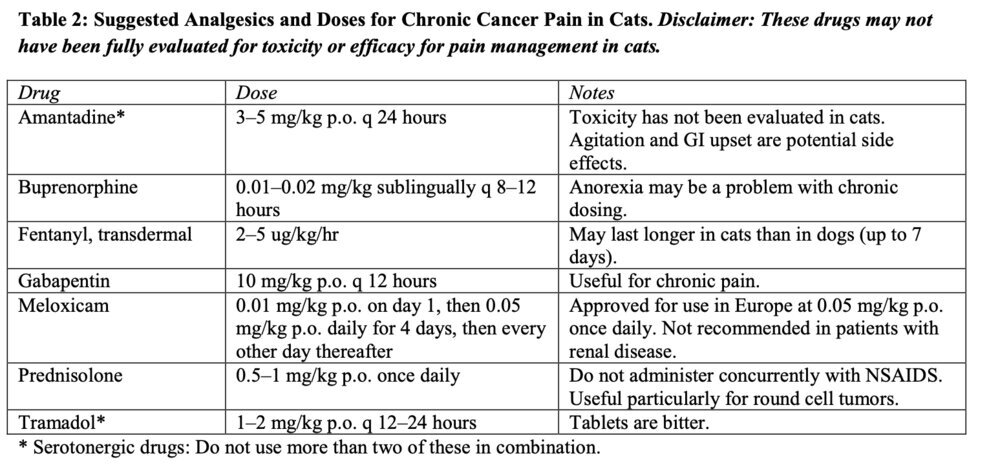
Tables 1 and 2 list commonly utilized drugs for pain management in dogs and cats with cancer along with recommended doses. Disclaimer: Most of these drugs have not been fully evaluated for toxicity or efficacy when administered long-term to manage cancer pain. It is important to counsel clients on the risks of using these drugs.
Steroids
Steroids should never be used prior to obtaining a diagnosis, since they can both inhibit the ability to obtain a definitive diagnosis and induce drug resistance, which is a problem in dogs who go on to receive chemotherapy for their cancer. Steroids are particularly useful in managing discomfort associated with round cell tumors such as lymphoma, multiple myeloma, mast cell tumors, and histiocytic sarcoma. Steroids should not be used in combination with NSAIDS because gastrointestinal and hepatic toxicity is exacerbated with this combination. Prednisone upregulates p-glycoprotein and induces multidrug resistance and thus should not be used in patients whose owners are considering chemotherapy. Drug resistance and failure to respond to treatment are common in patients that have received prednisone treatment prior to starting chemotherapy.
Acupuncture
Currently there is limited data on the usefulness of acupuncture to alleviate pain in veterinary patients; however, in humans, it appears that this modality may be useful to help manage pain, and it is often inexpensive and safe. The author’s experience has been positive in helping some cancer patients with chronic pain utilizing acupuncture. Thus the author recommends considering this modality in cancer patients and evaluating their response. Typically, four weekly sessions are recommended as a trial period; if a patient has not responded to acupuncture in this time, it is unlikely the patient will benefit. Specific training is required, and patients should be referred to someone with this training and certification. Acupuncturists treating animals should be well trained in an understanding of animal health as well as in anatomy and physiology, particularly acupuncture anatomy and physiology. The following sites may be useful in helping you to find a veterinarian trained in acupuncture: International Veterinary Acupuncture Society, at , and the Chi Institute, (click “Find a Vet”).
Secondary Infections
Oral tumors, bladder tumors, and tumors that become ulcerated commonly become infected with secondary bacterial infections. Treating these infections can do wonders for the comfort level of cancer patients. In the oral cavity, anaerobic bacteria are often the culprits, and thus good antibiotics to consider in controlling oral tumor infections include amoxicillin/clavulanic acid, clindamycin, and metronidazole. Multidrug resistant infections are common in patients with urogenital tumors, and therefore urine culture and sensitivity is recommended to help you choose appropriate antibiotics in these patients. For patients with prostatic tumor involvement, be sure to consider the antibiotic’s ability to penetrate the prostate. Good choices include enrofloxacin, marbofloxacin, and potentiated sulfas such as trimethoprim-sulfa. Tumors of the skin and mammary gland that become ulcerated are often infected with E. coli and Staphylococcus species, and the cephalosporins and amoxicillin/clavulanic acid are often good antibiotic choices for infected tumors involving the skin.
Nutrition
Ensuring that cancer patients, particularly those with oral tumors, are receiving adequate nutrition is important. High-quality diets are recommended. There are several diets specifically formulated for patients with cancer; however, there is no evidence to support a change in survival in patients fed these diets. There is evidence that these diets may be useful in cancer patients who are underweight and potentially suffering from cancer cachexia.
Feeding tubes are not recommended by the author for veterinary cancer patients. Often when feeding tubes are required in veterinary patients, the patient’s quality of life has declined to a point where continued life is not in the best interest of the patient. Feeding tubes enable owners who may be having trouble letting go to continue to feed the patient and keep them alive long past the point where their quality of life is acceptable. It is the author’s opinion that euthanasia should be considered when cancer patients are unable or unwilling to eat.
Preparing Clients for Euthanasia
Research suggests that 70% of pet owners are affected emotionally by the death of a pet, with 30% of these clients experiencing severe grief in anticipation of the loss of their pets. One of the hardest decisions for clients to make is: “When is the correct time to euthanize?” Many pet owners rely on their veterinarians to make the recommendation or give them permission for euthanasia, and thus it is critical for the veterinarian to have this conversation. Clients may be concerned that they are “giving up” on their pets and may need assurance that euthanasia is a valid, humane, and selfless decision. Some suggested ways to word these conversations include:
• “It is important for us to discuss hospice care and the option of euthanasia as Max declines...”
• “I know it is hard to consider letting Rover go, but euthanasia is a humane, selfless option for you to consider in alleviating his pain and suffering...”
• “Euthanasia is a humane option for Belle in light of how the cancer has spread…
Creating a designated end-of-life plan and discussing the option of euthanasia is critical in preparing the client for these steps. Having a plan in place can make the last visit easier on both the client and the veterinary team.
Table 1: Suggested Analgesics and Doses for Chronic Cancer Pain in Dogs. Disclaimer: These drugs may not have been fully evaluated for toxicity or efficacy for pain management in dogs.
Selected References
Adams CL, Bonnett BN, Meek AH. Predictors of owner response to companion animal death in 177 clients from 14 practices in Ontario. J Am Vet Med Assoc 2000;217:1303–1309.
Henry CJ, Higginbotham ML. Cancer management in small animal practice. St. Louis: Saunders Elsevier, 2010. Plumb DC. Plumb’s veterinary drug handbook, 7th ed. Stockholm, WI: PharmaVet, 2011.
Shaw JR, Legoni L. End-of-life communication in veterinary medicine: delivering bad news and euthanasia decision making. Vet Clin Small Anim Pract 2007;37:95.
Withrow SJ, Vail DM, Page RL. Withrow & MacEwen’s small animal clinical oncology, 5th ed. St. Louis: Elsevier, 2012.
The author would like to thank Dr. Ralph Harvey for his input on this topic.

by Sara Allstadt Frazier, DVM, Diplomate ACVIM (Oncology)
Approximately half of senior-aged dogs and one-third of cats will die of cancer, and thus it is likely that the general practitioner will have to manage patients with cancer. Regardless of the treatment options chosen, the patient’s comfort level is most important when managing cancer. The incidence of pain associated with cancer in humans is reported to be as high as 90%, and while such data is not available for dogs, some estimates suggest that roughly 50% of cancer-bearing dogs experience pain. In the author’s experience, tumors that most likely cause pain and discomfort include tumors of the bone, oral cavity, urogenital tract, head (particularly ocular and nasal tumors), and gastrointestinal tract, as well as those tumors that affect nerves or nerve roots. Additionally, tumors that become ulcerated also appear to cause significant discomfort. This is a brief review of palliative care options, most of which can be utilized in the general practice setting. The goal of palliative care is to achieve the best quality of life for patients and their families.
Assessment of Pain
Assessment of pain in veterinary patients can be a challenge and it is important to use a “team approach” to pain assessment in our patients. First, assess the patient and look at the patient’s interaction and behavior with its owners, with you, and with your staff. Is the patient guarding the affected area? Is the patient reluctant to move and interact? Is the patient’s attitude and interaction normal, based on past experience with that pet? Then, perform your physical exam and assess palpation-induced pain. Ask your team members who know the pet well for their thoughts on how the pet is doing. Then, quiz the owner on the day-to-day activity of the pet, the pet’s ability to ambulate well, the pet’s quality of sleep and appetite, and the pet’s participation in favorite activities.
Sometimes owners have a hard time seeing slow, day-to-day declines in their pets that may be more obvious to the veterinary team. One useful question to ask is, “What are your dog’s three favorite things?” Favorite activities may be greeting the owner at the door, eating, chasing a ball or other toy, or playing with the family. Ask if the pet is still active in these things. If not, then this is a sign that the patient’s quality of life may not be optimal.
Pain Management
Tumors that commonly cause pain include oral tumors, bone tumors, nerve sheath tumors (particularly those that affect the brachial plexus), nasal tumors, ocular tumors, urogenital tumors, pancreatic and gastrointestinal tumors, and ulcerated skin tumors. The author strongly recommends starting a pain management regimen as soon as tumors in these locations are diagnosed, as early intervention leads to better control of pain.
Generally, starting with a nonsteroidal anti-inflammatory drug (NSAID) is recommended. For tumors affecting bone, often an NSAID alone is not sufficient, and the addition of tramadol, gabapentin, and/or amantadine may be indicated. Bisphosphonates should also be considered in patients with osteolytic bone lesions, although further study is required to fully characterize the usefulness of this class of drug for pain management. The author has observed several patients who benefited significantly from treatment with this class of drugs; thus, it may be worthwhile trying a course in dogs with bone lesions.
In dogs with oral squamous cell carcinoma (OSCC), complete responses have been documented to piroxicam alone, and therefore this NSAID is recommended to manage this particular tumor. In cats with OSCC, meloxicam is recommended due to the poor pharmacokinetics of piroxicam in cats. Owners should be cautioned about the risk of nephrotoxicity with both of these drugs; however, given the short expected survival times in these cats, renal toxicity is often not the life-limiting factor. Additional pain medications are often required to alleviate bone pain. Many dogs and cats are successful in hiding their pain, and owners and veterinarians alike may be challenged to recognize the symptoms of pain in these patients.
Radiation Therapy
A palliative course of radiation therapy is often very useful for managing bone pain. For primary bone tumors such as osteosarcoma, approximately three out of four patients will experience some alleviation of pain in response to radiation therapy. Oral tumors commonly shrink with radiation therapy, and thus both pain relief and reduction of the physical mass may be achieved with this modality. Often, palliative courses of radiation therapy are administered once a week for a total of four weeks, although other courses may be recommended, depending on the tumor type and location. Round cell tumors such as histiocytic sarcoma or multiple myeloma commonly affect bone and typically respond very favorably to radiation.
Combination Therapy
Combination therapy is recommended in most cancer patients, as it is unlikely that any one drug will alleviate all pain associated with cancer. The author typically starts with an NSAID and tramadol, adding in gabapentin, Tylenol 3 or 4 (in dogs only), or amantadine as needed. Gabapentin and amantadine seem to be particularly useful to manage neuropathic pain. Caution should be used when combining drugs that affect the serotonergic system (tramadol, amantadine, amitriptyline, mirtazapine); it is recommended to not use more than two of these in combination.
Tables 1 and 2 list commonly utilized drugs for pain management in dogs and cats with cancer along with recommended doses. Disclaimer: Most of these drugs have not been fully evaluated for toxicity or efficacy when administered long-term to manage cancer pain. It is important to counsel clients on the risks of using these drugs.
Steroids
Steroids should never be used prior to obtaining a diagnosis, since they can both inhibit the ability to obtain a definitive diagnosis and induce drug resistance, which is a problem in dogs who go on to receive chemotherapy for their cancer. Steroids are particularly useful in managing discomfort associated with round cell tumors such as lymphoma, multiple myeloma, mast cell tumors, and histiocytic sarcoma. Steroids should not be used in combination with NSAIDS because gastrointestinal and hepatic toxicity is exacerbated with this combination. Prednisone upregulates p-glycoprotein and induces multidrug resistance and thus should not be used in patients whose owners are considering chemotherapy. Drug resistance and failure to respond to treatment are common in patients that have received prednisone treatment prior to starting chemotherapy.
Acupuncture
Currently there is limited data on the usefulness of acupuncture to alleviate pain in veterinary patients; however, in humans, it appears that this modality may be useful to help manage pain, and it is often inexpensive and safe. The author’s experience has been positive in helping some cancer patients with chronic pain utilizing acupuncture. Thus the author recommends considering this modality in cancer patients and evaluating their response. Typically, four weekly sessions are recommended as a trial period; if a patient has not responded to acupuncture in this time, it is unlikely the patient will benefit. Specific training is required, and patients should be referred to someone with this training and certification. Acupuncturists treating animals should be well trained in an understanding of animal health as well as in anatomy and physiology, particularly acupuncture anatomy and physiology. The following sites may be useful in helping you to find a veterinarian trained in acupuncture: International Veterinary Acupuncture Society, at , and the Chi Institute, (click “Find a Vet”).
Secondary Infections
Oral tumors, bladder tumors, and tumors that become ulcerated commonly become infected with secondary bacterial infections. Treating these infections can do wonders for the comfort level of cancer patients. In the oral cavity, anaerobic bacteria are often the culprits, and thus good antibiotics to consider in controlling oral tumor infections include amoxicillin/clavulanic acid, clindamycin, and metronidazole. Multidrug resistant infections are common in patients with urogenital tumors, and therefore urine culture and sensitivity is recommended to help you choose appropriate antibiotics in these patients. For patients with prostatic tumor involvement, be sure to consider the antibiotic’s ability to penetrate the prostate. Good choices include enrofloxacin, marbofloxacin, and potentiated sulfas such as trimethoprim-sulfa. Tumors of the skin and mammary gland that become ulcerated are often infected with E. coli and Staphylococcus species, and the cephalosporins and amoxicillin/clavulanic acid are often good antibiotic choices for infected tumors involving the skin.
Nutrition
Ensuring that cancer patients, particularly those with oral tumors, are receiving adequate nutrition is important. High-quality diets are recommended. There are several diets specifically formulated for patients with cancer; however, there is no evidence to support a change in survival in patients fed these diets. There is evidence that these diets may be useful in cancer patients who are underweight and potentially suffering from cancer cachexia.
Feeding tubes are not recommended by the author for veterinary cancer patients. Often when feeding tubes are required in veterinary patients, the patient’s quality of life has declined to a point where continued life is not in the best interest of the patient. Feeding tubes enable owners who may be having trouble letting go to continue to feed the patient and keep them alive long past the point where their quality of life is acceptable. It is the author’s opinion that euthanasia should be considered when cancer patients are unable or unwilling to eat.
Preparing Clients for Euthanasia
Research suggests that 70% of pet owners are affected emotionally by the death of a pet, with 30% of these clients experiencing severe grief in anticipation of the loss of their pets. One of the hardest decisions for clients to make is: “When is the correct time to euthanize?” Many pet owners rely on their veterinarians to make the recommendation or give them permission for euthanasia, and thus it is critical for the veterinarian to have this conversation. Clients may be concerned that they are “giving up” on their pets and may need assurance that euthanasia is a valid, humane, and selfless decision. Some suggested ways to word these conversations include:
• “It is important for us to discuss hospice care and the option of euthanasia as Max declines...”
• “I know it is hard to consider letting Rover go, but euthanasia is a humane, selfless option for you to consider in alleviating his pain and suffering...”
• “Euthanasia is a humane option for Belle in light of how the cancer has spread…
Creating a designated end-of-life plan and discussing the option of euthanasia is critical in preparing the client for these steps. Having a plan in place can make the last visit easier on both the client and the veterinary team.
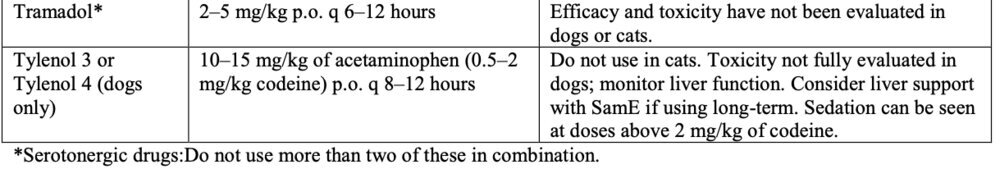
Table 1: Suggested Analgesics and Doses for Chronic Cancer Pain in Dogs. Disclaimer: These drugs may not have been fully evaluated for toxicity or efficacy for pain management in dogs.
| Drug | Dose | Notes |
| Amantadine* | 4–5 mg/kg p.o. once daily | Useful for neuropathic pain in humans, particularly in combination with NSAIDs. GI effects may be seen in first few days at higher doses, such as loose stools and gas. Caution when using other serotonergic drugs. |
| Fentanyl | 2–5 mcg/hr transdermal patch | Transdermal patches require changing approximately every 3 to 4 days, thus limited usefulness for long-term control. |
| Gabapentin | 3–10 mg/kg p.o. q 6–12 hours | May sedate; however, sedation effect usually lessens over the first week of administration. Not well evaluated in dogs as an analgesic. |
| NSAIDs | Piroxicam 0.3 mg/kg p.o. once daily with food | Do not use in patients with renal disease. Monitor renal function closely. Do not dose 0.3 mg/kg. GI upset reported; may be alleviated with famotidine, omeprazole, or misoprostil (however, misoprostil commonly causes GI cramping). |
| Carprofen 2.2 mg/kg p.o. q 12 hours | GI upset and adverse renal and hepatic effects possible. | |
| Meloxicam 0.2 mg/kg p.o. once, then 0.1 mg/kg p.o. q 24 hours with food | GI upset and adverse renal and hepatic effects possible. | |
| Deracoxib 1–2 mg/kg p.o. once daily | GI upset and adverse renal and hepatic effects possible; alternative to piroxicam for urinary bladder TCC. | |
| Firocoxib 5 mg/kg p.o. once daily | GI upset and adverse renal and hepatic effects possible; highly protein bound, so take caution when using with other anti-inflammatory agents, sulfonamides, and other protein-bound drugs. | |
| Pamidronate | 1–2 mg/kg IV diluted in 250 mL, or 4 mL/kg of saline administered over 2 hours as an infusion | Inhibits breakdown of bone through inhibition of osteoclasts. May take days to weeks to see effects. May be repeated every 4 weeks. |
| Prednisone | 0.25–1 mg/kg p.o. q 12–24 hours | Do not administer concurrently with NSAIDS. Useful particularly for round cell tumors. Upregulates p-glycoprotein in dogs and causes multidrug resistance; do not use in patients where client may be interested in additional treatment |
Selected References
Adams CL, Bonnett BN, Meek AH. Predictors of owner response to companion animal death in 177 clients from 14 practices in Ontario. J Am Vet Med Assoc 2000;217:1303–1309.
Henry CJ, Higginbotham ML. Cancer management in small animal practice. St. Louis: Saunders Elsevier, 2010. Plumb DC. Plumb’s veterinary drug handbook, 7th ed. Stockholm, WI: PharmaVet, 2011.
Shaw JR, Legoni L. End-of-life communication in veterinary medicine: delivering bad news and euthanasia decision making. Vet Clin Small Anim Pract 2007;37:95.
Withrow SJ, Vail DM, Page RL. Withrow & MacEwen’s small animal clinical oncology, 5th ed. St. Louis: Elsevier, 2012.
The author would like to thank Dr. Ralph Harvey for his input on this topic.