David Baxter PhD
Late Founder
Weight Loss Surgery and Eating Disorders
by Joanne Poppink, MFT, EatingDisorderRecovery.net
October 14, 2017
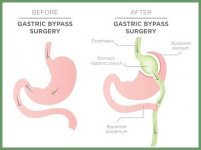
Mirror Mirror is running an excellent factual article describing weight loss surgery: Weight Loss Surgery and Eating Disorders.
In my experience as an eating disorder recovery psychotherapist I've seen tragic outcomes from weight loss surgery. Yes, I grant that it's possible, for a person without an eating disorder, to reap medical benefits from the surgery. Weight loss does occur and can be helpful in health management.
But I've seen people with eating disorders deny their eating disorder symptoms, get the surgery, suffer from the pain and life limiting diarrhea, get emotionally high from the weight loss and then eat their way back to obesity with even more medical challenges. What's worse, their anger and shame after going through this heart breaking journey causes them to reject new psychological help.
The dilemma is that an obese person with an eating disorder may believe that weight is the cause of their life problems and therefore, weight loss will bring them the life of their dreams. They don't factor in the reality of the eating disorder itself. So when weight loss does come from a mechanical intervention, the psychological, emotional and spiritual inner challenges are untouched.
Those challenges were softened or numbed by eating and carrying excess weight. And the eating and weight return to care for the suddenly exposed person who no longer carries the excess weight - excess in terms of health and cultural standards but not excess in terms of psychological protection.
The healing journey is complex, deep, thorough and results in a lasting healthy presence in the world. As much as we might wish it, there are no shortcuts. In fact, shortcuts can undermine your healing path.
Joanna Poppink, MFT, created this site. Joanna is a Los Angeles psychotherapist, speaker and author of Healing Your Hungry Heart: Recovering from your eating disorder. She specializes in eating disorder recovery for adult women and with an emphasis on building a fulfilling life beyond recovery.
To make contact with Joanna for an in-person appointment at her West Los Angeles office or to invite her to speak to your organization or for a free telephone or Skype consultation, please e-mail her at: joanna@poppink.com or call 310-474-4165.
by Joanne Poppink, MFT, EatingDisorderRecovery.net
October 14, 2017
Mirror Mirror is running an excellent factual article describing weight loss surgery: Weight Loss Surgery and Eating Disorders.
In my experience as an eating disorder recovery psychotherapist I've seen tragic outcomes from weight loss surgery. Yes, I grant that it's possible, for a person without an eating disorder, to reap medical benefits from the surgery. Weight loss does occur and can be helpful in health management.
But I've seen people with eating disorders deny their eating disorder symptoms, get the surgery, suffer from the pain and life limiting diarrhea, get emotionally high from the weight loss and then eat their way back to obesity with even more medical challenges. What's worse, their anger and shame after going through this heart breaking journey causes them to reject new psychological help.
The dilemma is that an obese person with an eating disorder may believe that weight is the cause of their life problems and therefore, weight loss will bring them the life of their dreams. They don't factor in the reality of the eating disorder itself. So when weight loss does come from a mechanical intervention, the psychological, emotional and spiritual inner challenges are untouched.
Those challenges were softened or numbed by eating and carrying excess weight. And the eating and weight return to care for the suddenly exposed person who no longer carries the excess weight - excess in terms of health and cultural standards but not excess in terms of psychological protection.
The healing journey is complex, deep, thorough and results in a lasting healthy presence in the world. As much as we might wish it, there are no shortcuts. In fact, shortcuts can undermine your healing path.
Joanna Poppink, MFT, created this site. Joanna is a Los Angeles psychotherapist, speaker and author of Healing Your Hungry Heart: Recovering from your eating disorder. She specializes in eating disorder recovery for adult women and with an emphasis on building a fulfilling life beyond recovery.
To make contact with Joanna for an in-person appointment at her West Los Angeles office or to invite her to speak to your organization or for a free telephone or Skype consultation, please e-mail her at: joanna@poppink.com or call 310-474-4165.