Brain scans reveal why it is so difficult to recover from OCD and hint at ways forward
by Annemieke Apergis-Schoute
The Conversation
March 7, 2017
We often refer to people who are extremely neat or organised as “a bit OCD”. But the reality of living with obsessive compulsive disorder is a very different and serious matter.
People with the brain disorder struggle greatly with recurrent, intrusive thoughts (obsessions) and unwanted urges to repeat safety-seeking behaviours over and over again (compulsions). Common examples are exaggerated fears of contamination or causing injury – leading to excessive washing or checking. It is easy to see why that causes extreme distress and interferes with everyday life.
In some cases, people with OCD are tormented with agonising taboo thoughts, for example the fear that they will sexually abuse a child even though they have no desire whatsoever to do so. This is coupled with the compulsion to seek reassurance, for example by avoiding children or checking newspapers in case they have been accused. Such people are often too ashamed to disclose their symptoms, worrying about being punished or judged to be “insane”. When listening to such patients it is clear their torment is real, with day after day spent enduring irrational fears and repeating seemingly purposeless behaviours.
A standard treatment for OCD involves exposure and response prevention (ERP). This involves the patient confronting their worst fears while learning to not perform their compulsions. For example, it may include touching a toilet seat and not being allowed to wash your hands. This treatment is often combined with comparatively high doses of selective serotonin re-uptake inhibitor (SSRI) drugs – typically three times higher than that needed to treat depression. Together this can help many patients with OCD, but far from all. So why is OCD such a debilitating disorder and why can it be so hard to treat? Our new research offers a clue – and some hope for those struggling.
Naomi Fineberg, who leads a specialist clinic for patients with OCD, sees many for whom daily life is difficult and who continue to struggle with their disorder despite treatment. According to her, about 40% of patients fail to respond to individually-tailored treatments. What’s more, many are left with residual troublesome symptoms such as continuing obsessive thoughts or relapse.
Such patients may still fall into depression and suicidal behaviour after treatment, becoming so overwhelmed by their obsessive compulsive behaviours that they end up neglecting their family, work, friends and health. OCD in its most severe form disrupts even the most basic self-care activities, such as eating or drinking – sometimes resulting in the need for long-term hospitalisation or residential care.
OCD on the brain
The new study from our team here at the University of Cambridge, published in the Proceedings of the National Academy of Sciences, is now beginning to show why this is. We compared 43 OCD patients with 35 healthy control participants in an experiment designed to investigate why patients with OCD struggle to learn that not performing their safety behaviours is in fact “safe”. We did this by examining their ability to flexibly adjust their reactions to changes in threat while inside an fMRI scanner, which measures brain activity by tracking changes in blood flow, at the Wolfson Brain Imaging Centre.
We showed the participants two angry faces, of which one was sometimes paired with a mild electric shock to the wrist, making it threatening. Recordings of tiny changes in sweat indicated when participants were expecting a shock. To test flexible updating of threat we also reversed the stimuli so that the “safe” face became the threatening one and vice versa. The experiment tests the individual’s ability to learn when a stimulus is safe and so not to expect a shock. By reversing the stimuli, we introduced ambiguity as both faces had by then been associated with the possibility of a shock.

Ventromedial prefrontal cortex: signals safety.
Patrick J. Lynch, medical illustrator, CC BY-SA
Patients with OCD could initially learn which face predicted threat. But once this had been reversed they were unable to differentiate between the new and the old threatening stimulus – they treated both as threatening. We think this is because they never really learned that one of the faces was truly safe – something which was reflected in their brain activity. Unlike in the healthy participants, there was no signal from the OCD patients’ ventromedial prefrontal cortex, a brain area that normally signals safety.
The results suggest that OCD patients are likely to have difficulty learning when situations are safe in everyday life – and that this has to do with differences in the brain. This has great relevance for the current psychological treatment of OCD, in which patients are expected to learn that not performing excessive and compulsive safety behaviours is in fact “safe” and therefore unnecessary. Current exposure therapies may only teach patients how to deal with their compulsions rather than truly learning that the situations they are so scared of are not actually dangerous. This means that obsessive thoughts can persist, and that it is possible for compulsive behaviour to return in future stressful situations.
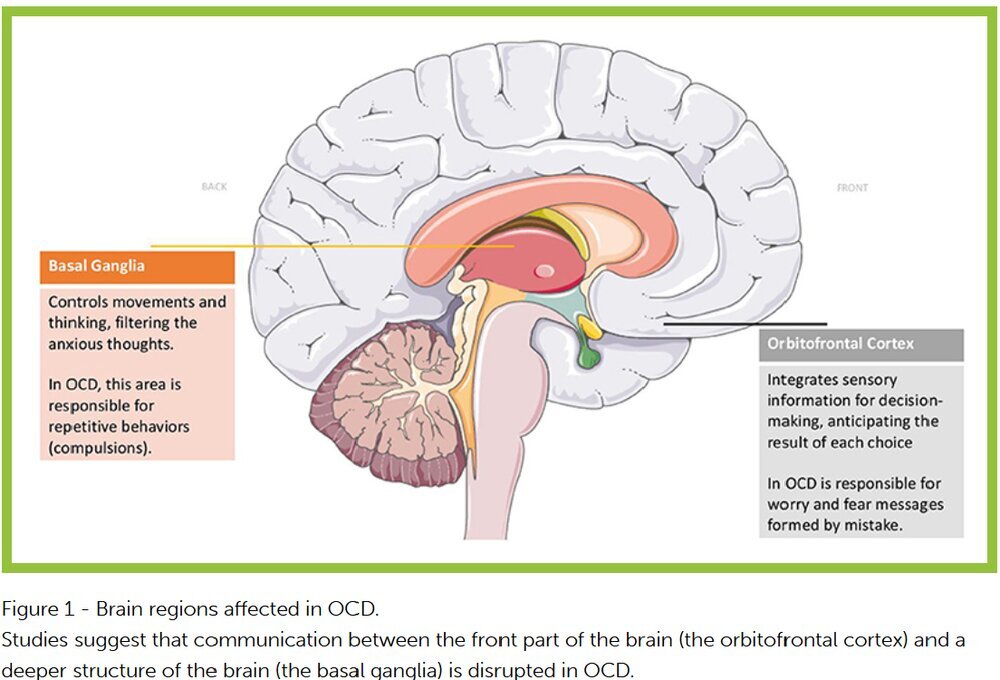
The research follows another recent study published in Biological Psychiatry, which discovered a lack of communication between specific brain areas in patients with OCD. In particular, it found disrupted connectivity between neural pathways that connect the front of the brain with the basal ganglia, which are critical for flexible thinking and goal-directed behaviours that we know are impaired in OCD patients and are likely to contribute to the difficulty of overcoming the drive to perform needless compulsions.
An avenue for improving future treatment for OCD would be to explore better learning in patients that not performing compulsive safety behaviours is truly safe. This could be achieved by boosting rewards in therapy for not performing safety behaviour or possibly with the help of certain drugs that can enhance the positive experience of not having to perform the compulsions.
by Annemieke Apergis-Schoute
The Conversation
March 7, 2017
We often refer to people who are extremely neat or organised as “a bit OCD”. But the reality of living with obsessive compulsive disorder is a very different and serious matter.
People with the brain disorder struggle greatly with recurrent, intrusive thoughts (obsessions) and unwanted urges to repeat safety-seeking behaviours over and over again (compulsions). Common examples are exaggerated fears of contamination or causing injury – leading to excessive washing or checking. It is easy to see why that causes extreme distress and interferes with everyday life.
In some cases, people with OCD are tormented with agonising taboo thoughts, for example the fear that they will sexually abuse a child even though they have no desire whatsoever to do so. This is coupled with the compulsion to seek reassurance, for example by avoiding children or checking newspapers in case they have been accused. Such people are often too ashamed to disclose their symptoms, worrying about being punished or judged to be “insane”. When listening to such patients it is clear their torment is real, with day after day spent enduring irrational fears and repeating seemingly purposeless behaviours.
A standard treatment for OCD involves exposure and response prevention (ERP). This involves the patient confronting their worst fears while learning to not perform their compulsions. For example, it may include touching a toilet seat and not being allowed to wash your hands. This treatment is often combined with comparatively high doses of selective serotonin re-uptake inhibitor (SSRI) drugs – typically three times higher than that needed to treat depression. Together this can help many patients with OCD, but far from all. So why is OCD such a debilitating disorder and why can it be so hard to treat? Our new research offers a clue – and some hope for those struggling.
Naomi Fineberg, who leads a specialist clinic for patients with OCD, sees many for whom daily life is difficult and who continue to struggle with their disorder despite treatment. According to her, about 40% of patients fail to respond to individually-tailored treatments. What’s more, many are left with residual troublesome symptoms such as continuing obsessive thoughts or relapse.
Such patients may still fall into depression and suicidal behaviour after treatment, becoming so overwhelmed by their obsessive compulsive behaviours that they end up neglecting their family, work, friends and health. OCD in its most severe form disrupts even the most basic self-care activities, such as eating or drinking – sometimes resulting in the need for long-term hospitalisation or residential care.
OCD on the brain
The new study from our team here at the University of Cambridge, published in the Proceedings of the National Academy of Sciences, is now beginning to show why this is. We compared 43 OCD patients with 35 healthy control participants in an experiment designed to investigate why patients with OCD struggle to learn that not performing their safety behaviours is in fact “safe”. We did this by examining their ability to flexibly adjust their reactions to changes in threat while inside an fMRI scanner, which measures brain activity by tracking changes in blood flow, at the Wolfson Brain Imaging Centre.
We showed the participants two angry faces, of which one was sometimes paired with a mild electric shock to the wrist, making it threatening. Recordings of tiny changes in sweat indicated when participants were expecting a shock. To test flexible updating of threat we also reversed the stimuli so that the “safe” face became the threatening one and vice versa. The experiment tests the individual’s ability to learn when a stimulus is safe and so not to expect a shock. By reversing the stimuli, we introduced ambiguity as both faces had by then been associated with the possibility of a shock.

Ventromedial prefrontal cortex: signals safety.
Patrick J. Lynch, medical illustrator, CC BY-SA
Patients with OCD could initially learn which face predicted threat. But once this had been reversed they were unable to differentiate between the new and the old threatening stimulus – they treated both as threatening. We think this is because they never really learned that one of the faces was truly safe – something which was reflected in their brain activity. Unlike in the healthy participants, there was no signal from the OCD patients’ ventromedial prefrontal cortex, a brain area that normally signals safety.
The results suggest that OCD patients are likely to have difficulty learning when situations are safe in everyday life – and that this has to do with differences in the brain. This has great relevance for the current psychological treatment of OCD, in which patients are expected to learn that not performing excessive and compulsive safety behaviours is in fact “safe” and therefore unnecessary. Current exposure therapies may only teach patients how to deal with their compulsions rather than truly learning that the situations they are so scared of are not actually dangerous. This means that obsessive thoughts can persist, and that it is possible for compulsive behaviour to return in future stressful situations.
The research follows another recent study published in Biological Psychiatry, which discovered a lack of communication between specific brain areas in patients with OCD. In particular, it found disrupted connectivity between neural pathways that connect the front of the brain with the basal ganglia, which are critical for flexible thinking and goal-directed behaviours that we know are impaired in OCD patients and are likely to contribute to the difficulty of overcoming the drive to perform needless compulsions.
An avenue for improving future treatment for OCD would be to explore better learning in patients that not performing compulsive safety behaviours is truly safe. This could be achieved by boosting rewards in therapy for not performing safety behaviour or possibly with the help of certain drugs that can enhance the positive experience of not having to perform the compulsions.