David Baxter PhD
Late Founder
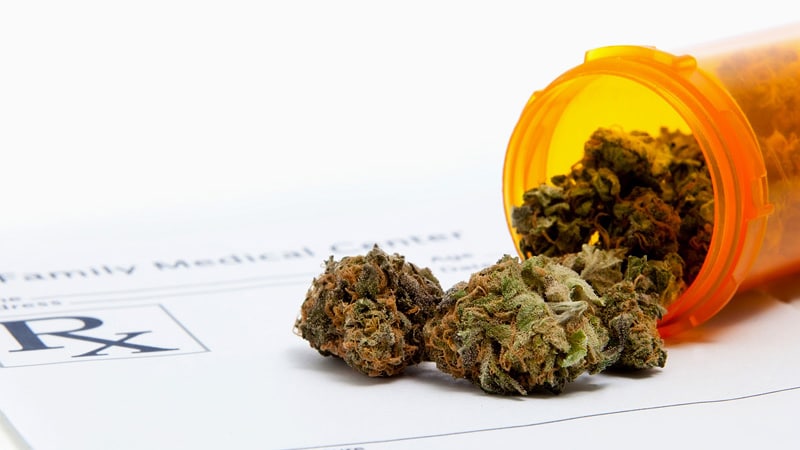
Medical Cannabis May Cut Opioid Use for Back Pain, OA
Preliminary data suggest more than one third of people with back pain no longer used opioids after filling cannabis prescriptions. Opioid prescriptions decreased as well for those with osteoarthritis.
March 28, 2022
Access to medical cannabis (MC) cut opioid prescriptions for patients with chronic non-cancer back pain and patients with osteoarthritis, according to preliminary data presented at the American Academy of Orthopaedic Surgeons (AAOS) 2022 Annual Meeting.
For those with chronic back pain, the average morphine milligram equivalents (MME) per day dropped from 15.1 to 11.0 (n = 186; P < .01). More than one third of the patients (38.7%) stopped taking morphine after they filled prescriptions for medical cannabis.
Opioid prescriptions were filled 6 months before access to MC and then were compared with 6 months after access to MC.
In analyzing subgroups, the researchers found that patients who started at less than 15 MME/day and more than 15 MME/day showed significant decreases after filling the MC prescription.
Almost half (48.5%) of the patients in the group that started at less than 15 MME daily dropped to 0 MME/day, and 13.5% of patients who were getting more than 15 MME/day stopped using opioids.
Data on filled opioid prescriptions was gathered from a Prescription Drug Monitoring Program (PDMP) system for patients diagnosed with chronic musculoskeletal non-cancer back pain who were eligible for MC access between February 2018 and July 2019.
Medical cannabis has shown benefit in treating chronic pain, but evidence has been limited on whether it can reduce opioid use, which can lead to substance abuse, addiction, overdose, and death, the researchers note.
Researchers found that using MC via multiple routes of administration seemed to be important.
Patients who used only a single administration route showed a statistically insignificant decrease in MME/day from 20.0 to 15.1 (n = 68; P = .054), whereas patients who used two or more routes showed a significant decrease from 13.2 to 9.5 (n = 76; P < .01).
Ari Greis, DO, a physical medicine and rehabilitation specialist in Bryn Mawr, Pennsylvania, and a co-author on the MC studies for both back pain and OA, told Medscape Medical News, "We have many patients who are benefiting from a single route of delivery for chronic orthopedic pain. However, our data shows a greater reduction in opioid consumption in patients using more than one route of delivery."
He said delivery modes in the studies included vaporized cannabis oil or flower; sublingual tinctures; capsules or tablets; and topical lotions, creams, and salves.
Greis is the director of the Medical Cannabis Department at Rothman Orthopaedic Institute and is a senior fellow in the Institute of Emerging Health Professions and the Lambert Center for the Study of Medicinal Cannabis and Hemp.
Medical Cannabis Also Reduces Opioids for OA
The same team of researchers, using the data from the PDMP system, showed that medical cannabis also helped reduce opioid use for osteoarthritis.For patients using opioids for OA, there was a significant decrease in average MME/day of prescriptions filled by patients following MC access — from 18.2 to
9.8 (n = 40; P < .05). The average drop in MME/day was 46.3%. The percentage of patients who stopped using opioids was 37.5%. Pain score on a 0 to 10 visual analog scale decreased significantly from 6.6 (n = 36) to 5.0 (n = 26; P < .01) at 3 months and 5.4 (n = 16; P < .05) at 6 months.
Gary Stewart, MD, an orthopedic surgeon in Morrow, Georgia, and member of the AAOS Opioid Task Force, who was not part of the studies, told Medscape Medical News that the studies offer good preliminary data to offer help with the opioid issue.
"I sometimes feel that we, as orthopedic surgeons and physicians in general, are working with one hand behind our back. We're taking something that is a heroin or morphine derivative and giving it to our patients when we know it has a high risk of building tolerance and addiction. But at the same time, we have no alternative," he said.
He said it's important to remember the results from the relatively small study are preliminary and observational. People used different forms and amounts of MC and the data show only that prescriptions were filled, but not whether the cannabis was used. Prospective, controlled studies where opioids go head-to-head with MC are needed, he said.
"Still, this can lead us to more studies to give us an option [apart from] an opioid that we know is highly addictive," he said.

:max_bytes(150000):strip_icc()/GettyImages-184315230-5a6a20f3eb97de001ac362d0.jpg)