The cheapest way to talk online to a board-certified vet oncologist (who is also a cancer researcher / assistant professor at Ohio State):

Dr. Megan Brown -Expert in Veterinary, Cat Veterinary, Dog Veterinary
Get expert answer from Dr. Megan Brown on a wide range of topics and questions: Veterinary, Cat Veterinary, Dog Veterinary and morewww.justanswer.com
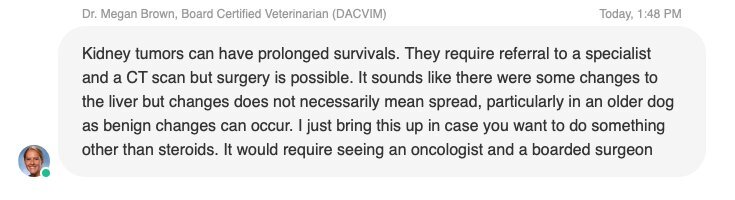
The oncologist, Dr. Brown, was very helpful in answering questions at JustAnswer about my elderly dog's kidney cancer. For one thing, she explained why my dog hasn't died yet. She confirmed my hunch that the cancer may not have spread to the liver. Unlike the primary care vets who were overly pessimistic about the prognosis (like he should have died two months ago), Dr. Brown says surgery is a possible option (though I am not going that route due to cost):
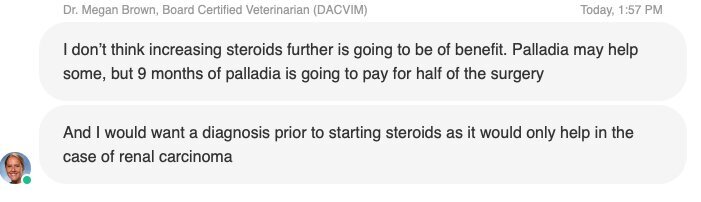
Also, there isn't any need to increase the steroid dose concerning the cancer itself. Palladia may help to some degree:
Here in Arizona, the cost for the surgery (a nephrectomy) is well over $4,000 USD, not including the cost of CT imaging, aftercare in the case of complications, etc. I have also read case reports where some of the dogs died soon after the surgery anyway, though that may have been due a lack of experience.
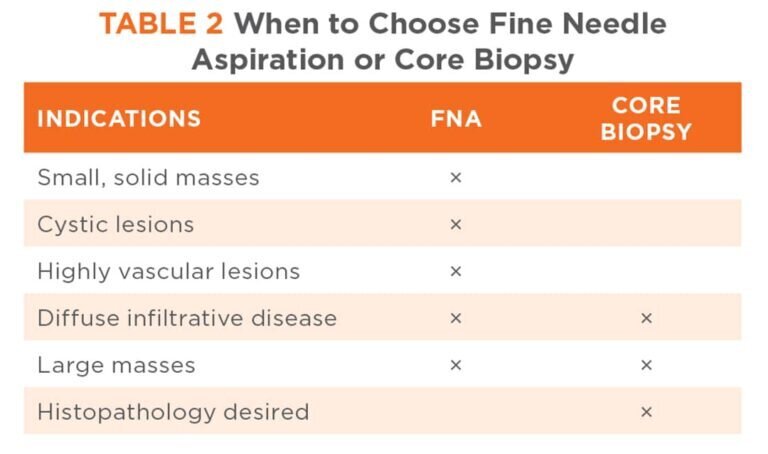
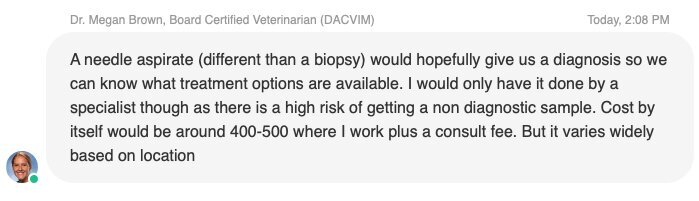
And a needle aspirate can be more expensive than I thought:
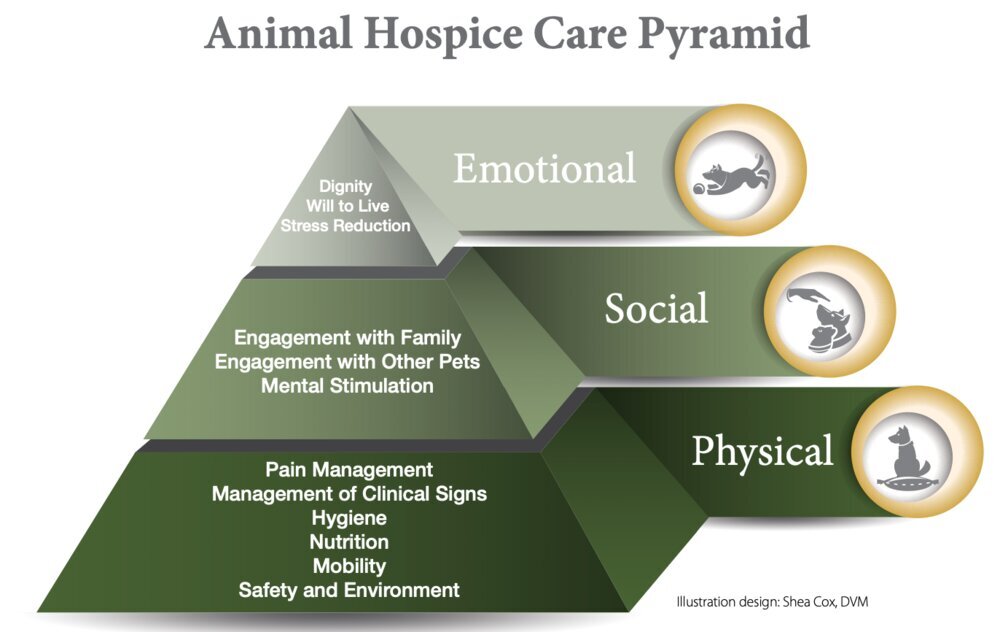
So, for now, instead of focusing on steroids or anything else as a potential solution, I am going to focus on just making the dog as happy as possible. I am still going with the relatively conservative route using NSAIDS or steroids (never both due to potentially deadly GI effects) along with gabapentin for any hidden pain, lots of toys and treats, low-dose marijuana tincture drops, nutritional and herbal supplements for overall health, and possibly frequent, basic bloodwork.
Last edited: