wheelchairdemon
Member
I have had severe spinal stenosis and severe disc degeneration for years. I'm in pain all the time. The doctor has been treating me with pain medication; hydromorphone to be exact.
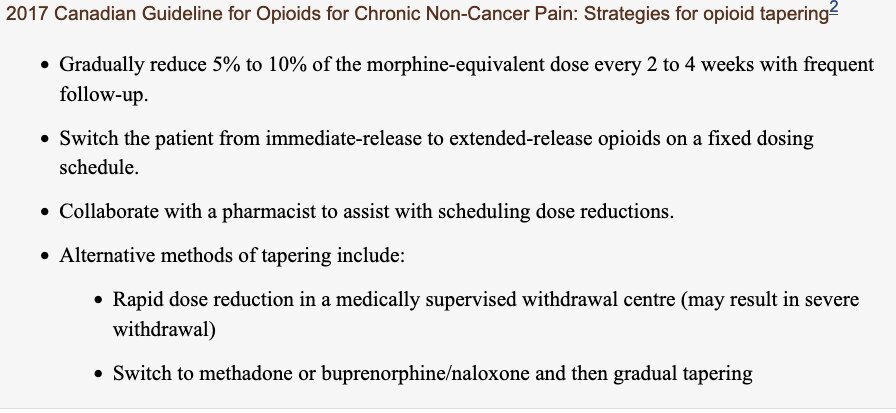
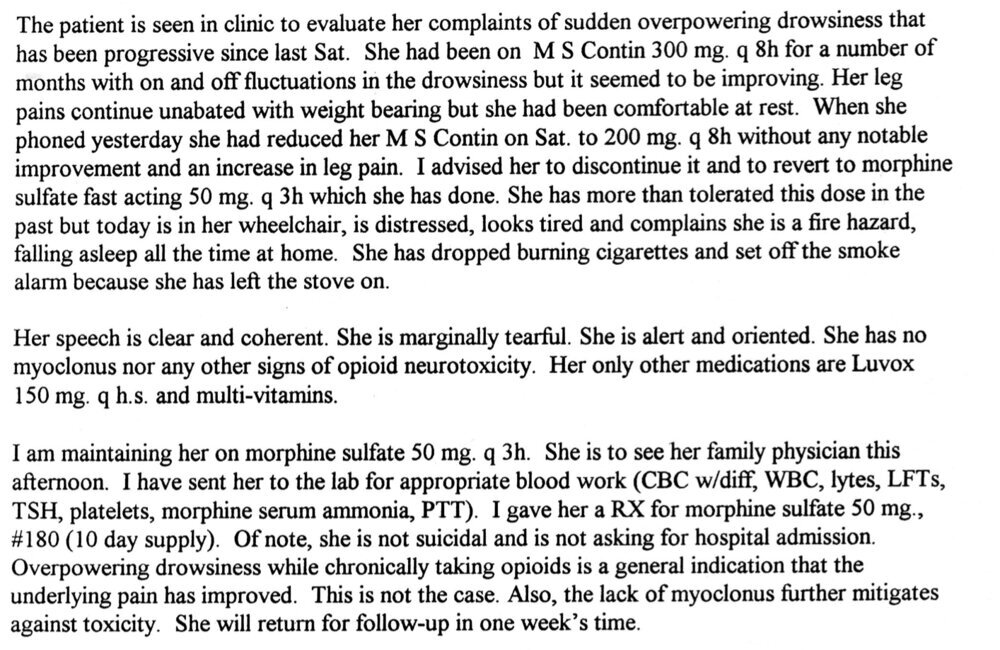
Two days ago my family doctor told me he must stop the pain medication. He's changing the policy in the clinic to a narcotics-free zone. He said chronic pain is a mental illness, not a physical problem. I asked him for a referral to a specialist who can help. He said he doesn't do that. He gave me one last prescription and told me it's up to me to figure out how to stop it. Can a person safely stop hydromorphone cold turkey?
I tried to get lower-dose tablets so I can slowly taper the dose down, but the doctor said he can't do that. None of this makes sense. With the pain properly managed I have a quality of life. I have not had to rely on the health care system for anything for many, many years. Instead, I'm active in Toastmasters, I sing in two choirs, I attend church, and I volunteer at the museum. I'm not happy about stopping the pain medication without an alternative method of treatment, but that's apparently what I have to do. I dread going back into the despairing feeling I had the last time the pain was out of control....
Anyway, tips on how to stop the pain medications without shocking my system badly, are welcome.
Two days ago my family doctor told me he must stop the pain medication. He's changing the policy in the clinic to a narcotics-free zone. He said chronic pain is a mental illness, not a physical problem. I asked him for a referral to a specialist who can help. He said he doesn't do that. He gave me one last prescription and told me it's up to me to figure out how to stop it. Can a person safely stop hydromorphone cold turkey?
I tried to get lower-dose tablets so I can slowly taper the dose down, but the doctor said he can't do that. None of this makes sense. With the pain properly managed I have a quality of life. I have not had to rely on the health care system for anything for many, many years. Instead, I'm active in Toastmasters, I sing in two choirs, I attend church, and I volunteer at the museum. I'm not happy about stopping the pain medication without an alternative method of treatment, but that's apparently what I have to do. I dread going back into the despairing feeling I had the last time the pain was out of control....
Anyway, tips on how to stop the pain medications without shocking my system badly, are welcome.