David Baxter PhD
Late Founder
Understanding Schizophrenia: Causes and Risk Factors
SchizophreniaConnection.com
December 26, 2006
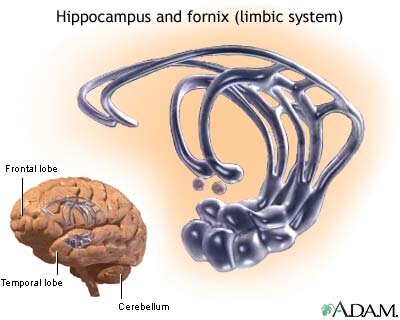
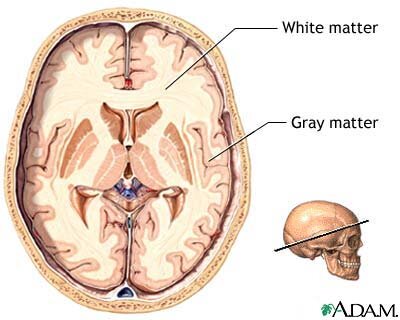
Schizophrenia is a group of psychotic disorders that interfere with thinking and responsiveness. It is a disease of the brain, just like Alzheimer's and Parkinson's diseases. The term schizophrenia, which means "split mind," was first used in 1911 by Swiss psychiatrist Eugen Bleuler to categorize patients whose thought processes and emotional responses seemed disconnected. Despite its name, the condition does not cause a split personality.
Schizophrenia is a group of psychotic disorders characterized by disturbances in perception, behavior, and communication that last longer than 6 months. (This includes psychotic behavior.) A person with schizophrenia has deteriorated occupational, interpersonal, and self-supportive abilities.
Schizophrenia is characterized by the following symptoms:
The disease is complicated by the fact that although a schizophrenic patient may have more than one symptom, he or she rarely has all of them. Symptoms also often go into remission.
Negative Symptoms
A person with schizophrenia may have the following negative symptoms:
Psychotic Symptoms
Psychotic symptoms, particularly delusions and hallucinations, are the most widely recognized manifestations of schizophrenia.
Cognitive Impairment (Disordered Thinking)
The symptoms of cognitive impairment and disordered thinking may occur before other symptoms of schizophrenia. They include:
Other Symptoms
People with schizophrenia may experience other symptoms such as intolerance of heat (often associated with antipsychotic medications) and a reduced sense of smell.
SchizophreniaConnection.com
December 26, 2006
Schizophrenia is a group of psychotic disorders that interfere with thinking and responsiveness. It is a disease of the brain, just like Alzheimer's and Parkinson's diseases. The term schizophrenia, which means "split mind," was first used in 1911 by Swiss psychiatrist Eugen Bleuler to categorize patients whose thought processes and emotional responses seemed disconnected. Despite its name, the condition does not cause a split personality.
Schizophrenia is a group of psychotic disorders characterized by disturbances in perception, behavior, and communication that last longer than 6 months. (This includes psychotic behavior.) A person with schizophrenia has deteriorated occupational, interpersonal, and self-supportive abilities.
Schizophrenia is characterized by the following symptoms:
- Delusions
- Hallucinations
- Disordered thinking
- Emotional unresponsiveness
- Negative symptoms (including apathy and social withdrawal)
- Psychotic symptoms
- Disordered thinking
The disease is complicated by the fact that although a schizophrenic patient may have more than one symptom, he or she rarely has all of them. Symptoms also often go into remission.
Negative Symptoms
A person with schizophrenia may have the following negative symptoms:
- Lack of self confidence
- Lack of emotions
- Colorless speaking tones
- Inappropriate reactions to events (such as laughing hysterically over a loss)
- A general loss of interest in life and the ability to experience pleasure
Psychotic Symptoms
Psychotic symptoms, particularly delusions and hallucinations, are the most widely recognized manifestations of schizophrenia.
- Hallucinations. A hallucination is the experience of seeing, hearing, tasting, smelling, or feeling something that doesn't really exist. Auditory hallucinations are false senses of sound such as hearing voices that go unheard by others. They are the most common psychotic symptoms, affecting about 70% of patients. One study reported that schizophrenic patients who had been profoundly deaf since birth were able to describe convincing experiences of hearing voices. Patients describe the voices as occurring all about them and that they are impossible to filter out or ignore.
- Delusions. A delusion is a fixed, false belief. It can be bizarre (such as invisible aliens have entered the room through an electric socket) or nonbizarre (such as unwarranted jealousy or the paranoid belief in being persecuted or watched).
Cognitive Impairment (Disordered Thinking)
The symptoms of cognitive impairment and disordered thinking may occur before other symptoms of schizophrenia. They include:
- A lack of attention
- Impaired information processing and an aberrant association between words and ideas. Sometimes this condition is so extreme that speech becomes incoherent and is referred to as "word salad." Patients may connect words because of similarity of sound, rather than by meaning, a condition known as "clang associations."
- Memory impairment. In keeping with other aspects of disordered thinking, memory impairment in schizophrenia is likely to involve the inability to connect an event with its source into a complete and whole memory. For instance, a patient may recall and even feel a familiarity with a specific event but be unable to remember where, when, or how it took place.
- Backward masking dysfunction. This is a trait in which a distraction causes a person to forget a preceding event. It might be an important symptom and a marker of schizophrenia even in people with normal working memories. One test to diagnose this trait uses four letters on a computer screen. The screen goes blank, and another image, called a masking stimulus, appears (such as four broken letter fragments). After viewing the images, the patient is asked to type in the original letters. Both symptomatic and presymptomatic patients commonly have problems with this particular exercise.
Other Symptoms
People with schizophrenia may experience other symptoms such as intolerance of heat (often associated with antipsychotic medications) and a reduced sense of smell.