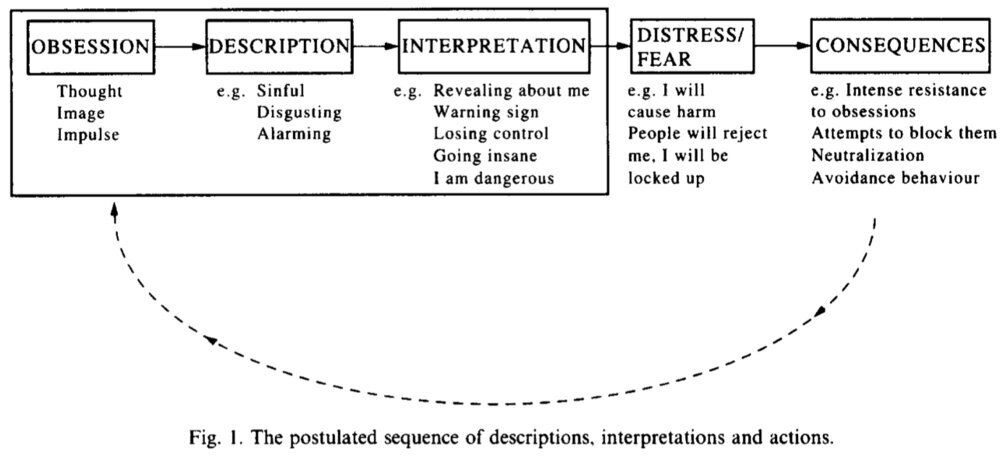
CBT (cognitive behavior therapy) involves actively challenging and confronting the distorted thinking and beliefs that drive and maintain obsessions and compulsions. Below are the key cognitive errors of people with OCD.
Black-and-White or All-or Nothing Thinking
Example: "If I’m not completely safe, then I’m in overwhelming danger."
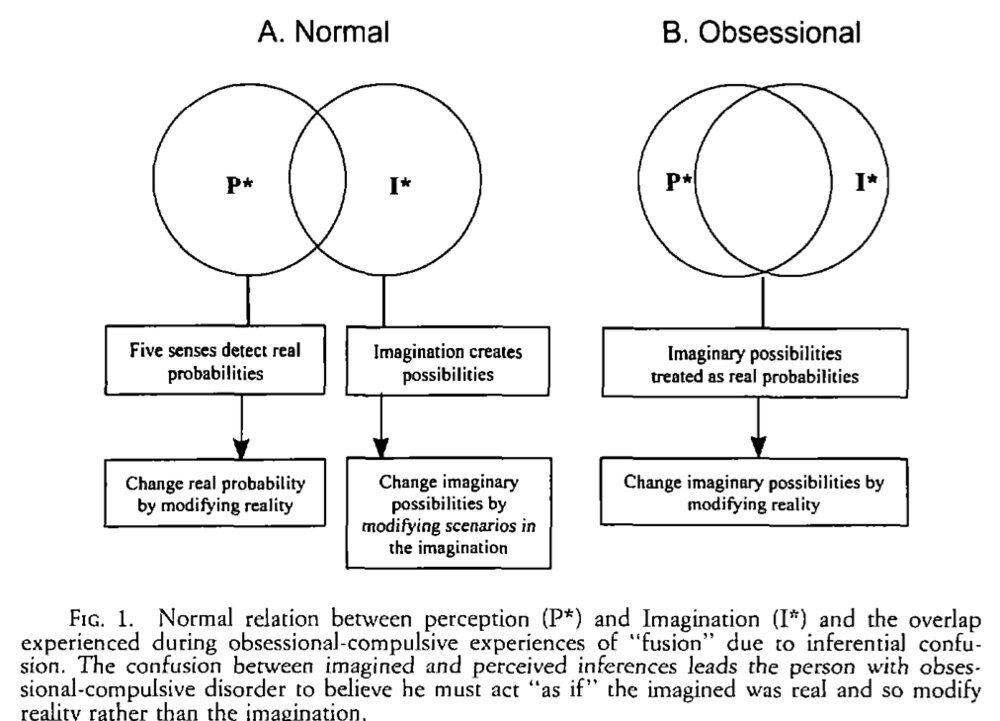
Magical Thinking
Example: "If I think bad thoughts, bad things will happen."
Overestimating Risk and Danger
Example: "If I take even a slight risk, I will come to great harm."
Perfectionism
Example: "I’ve got to do everything perfectly."
Hypermorality
Example: "I’ll be punished for every mistake."
Overresponsibility for Others
Example: "I must always guard against making mistakes that even remotely harm an innocent person."
Thought-Action Fusion (similar to Magical Thinking)
Example: "If I have a bad, even horrible thought about harming someone, it feels just as if I've actually done it or that it is highly likely to happen in the future."
Overimportance of Thought
Example: "If I think about a terrible event occurring, it is much more likely to happen."
Exclusivity Error
Example: "Bad things are much more likely to happen to me than to other people."
Martyr Complex
Example: "Suffering and sacrificing my life by doing endless rituals is a small price to pay to protect those I love. Since no harm has come to them, I must be doing something right."
“What If” Thinking
Example: "In the future, what if I...
do it wrong?"
make a mistake?"
get AIDS?"
am responsible for causing harm to someone?"
Intolerance of uncertainty
Example: "I can’t relax until I am 100% certain of everything and know everything will be OK."
Adapted from: The OCD Workbook: Your guide to breaking free from obsessive-compulsive disorder
Preview at: The OCD Workbook: Your guide to breaking free from obsessive-compulsive disorder
Black-and-White or All-or Nothing Thinking
Example: "If I’m not completely safe, then I’m in overwhelming danger."
Magical Thinking
Example: "If I think bad thoughts, bad things will happen."
Overestimating Risk and Danger
Example: "If I take even a slight risk, I will come to great harm."
Perfectionism
Example: "I’ve got to do everything perfectly."
Hypermorality
Example: "I’ll be punished for every mistake."
Overresponsibility for Others
Example: "I must always guard against making mistakes that even remotely harm an innocent person."
Thought-Action Fusion (similar to Magical Thinking)
Example: "If I have a bad, even horrible thought about harming someone, it feels just as if I've actually done it or that it is highly likely to happen in the future."
Overimportance of Thought
Example: "If I think about a terrible event occurring, it is much more likely to happen."
Exclusivity Error
Example: "Bad things are much more likely to happen to me than to other people."
Martyr Complex
Example: "Suffering and sacrificing my life by doing endless rituals is a small price to pay to protect those I love. Since no harm has come to them, I must be doing something right."
“What If” Thinking
Example: "In the future, what if I...
do it wrong?"
make a mistake?"
get AIDS?"
am responsible for causing harm to someone?"
Intolerance of uncertainty
Example: "I can’t relax until I am 100% certain of everything and know everything will be OK."
Adapted from: The OCD Workbook: Your guide to breaking free from obsessive-compulsive disorder
Preview at: The OCD Workbook: Your guide to breaking free from obsessive-compulsive disorder