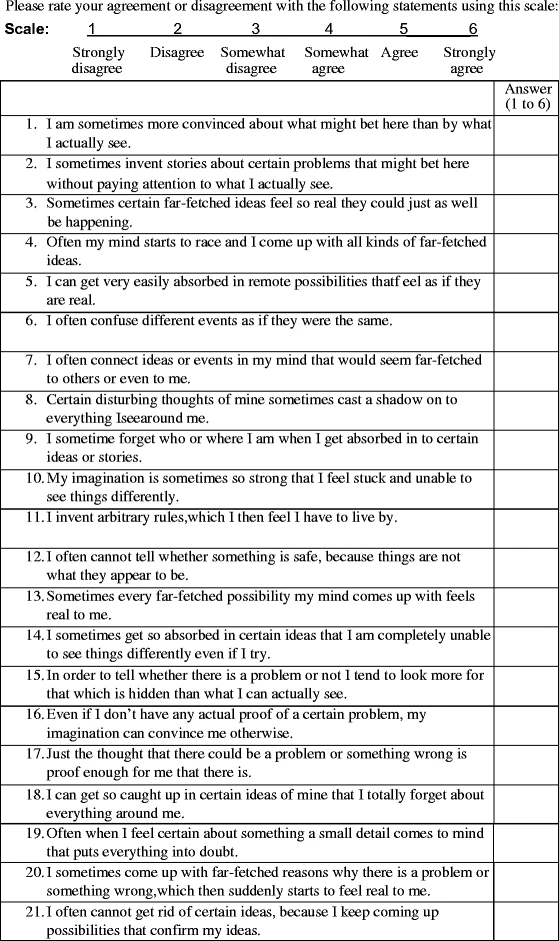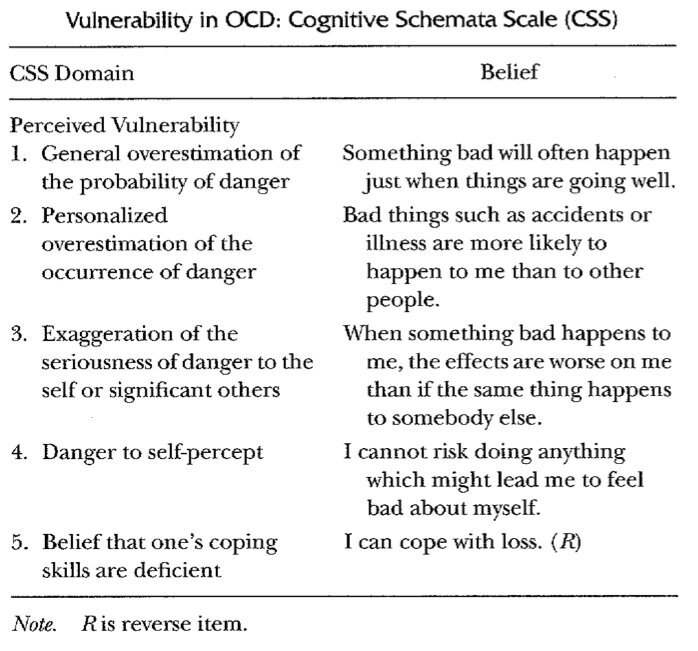
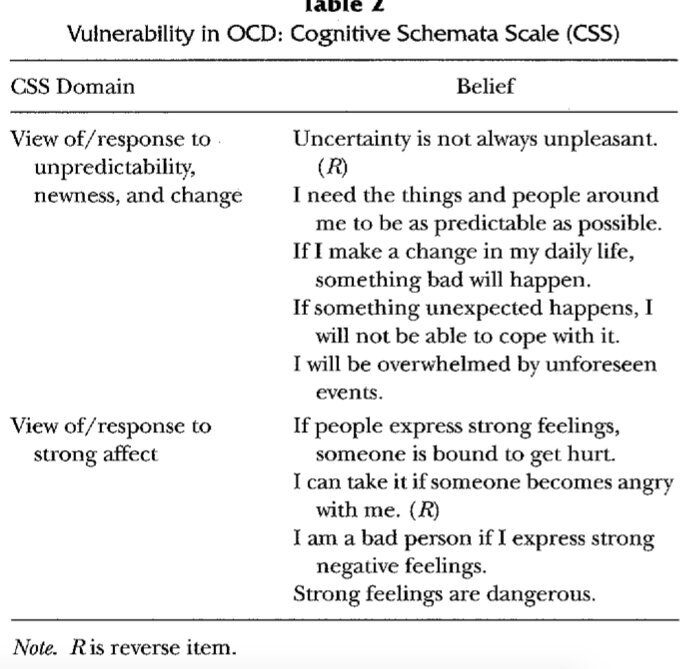
"...to address dysfunctional emotional beliefs, expressed as "I don't believe it's true, but I feel it's true." We hypothesize that in order to access and modify or mollify (make less salient, harsh, or destructive) a schema in treatment, the patient must become able to emotionally experience as well as to cognitively reflect upon its contents."
Last edited: